Disease Education Information
Early Diagnosis and Treatment Are Critical, but Elusive
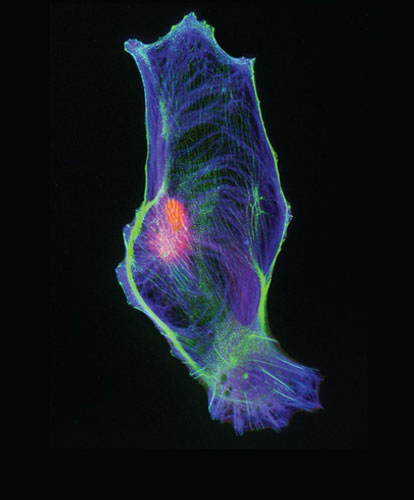
ATTR amyloidosis is a rare, progressive disease characterized by the abnormal buildup of amyloid deposits composed of misfolded transthyretin protein in the body’s organs and tissues.1,2 Because symptoms of ATTR amyloidosis are often similar to those of other diseases, the condition can be difficult to recognize and diagnose properly.3 However, ATTR amyloidosis is fatal if untreated, with a life-expectancy ranging between 3-15 years after the onset of symptoms, so early identification, diagnosis, and treatment are critical.4
- What is Transthyretin Amyloidosis (ATTR Amyloidosis)?
ATTR amyloidosis is a disease that can impact numerous organs and tissues in the body, including the peripheral nervous system, and organs such as the heart, kidneys, gastrointestinal tract, and eyes.2,5 Two primary presentations of ATTR amyloidosis are transthyretin amyloid polyneuropathy (ATTR-PN) and transthyretin amyloid cardiomyopathy (ATTR-CM).6
ATTR-PN results from a genetic mutation in the transthyretin gene, and amyloid fibrils deposit in the peripheral and autonomic nerves.7,8
In ATTR-CM, the abnormal buildup of amyloid deposits primarily occurs in the heart and is defined by restrictive cardiomyopathy and progressive heart failure.5
In both ATTR-PN and ATTR-CM, disease awareness is low and receiving an accurate diagnosis may be challenging, as symptoms are nonspecific or may be confused for other conditions.3,9,10 As awareness of the condition increases, and patient diagnosis improves, the medical community will have a better idea of how many people suffer from both forms of this rare disease.
- What is ATTR-PN?
Approximately 10,000, or 1.1 per 100,000 people in the world, are estimated to be living with ATTR-PN, although prevalence may be higher.11,12 The onset of ATTR-PN may occur in people as early as age thirty.7
AATTR-PN is hereditary13 and results from one of over 100 different mutations in the TTR gene that cause protein misfolding.14 Only one copy of the mutant gene is needed to transmit the disease, and an affected parent has a 50% chance of passing the mutation on to his or her children.13
Not everyone who inherits the mutant TTR gene will develop ATTR-PN.13 However, if symptoms of the disease are experienced, it is critical that individuals discuss them closely with doctors and family members. Physicians treating a patient with symptoms of the condition must examine the patient’s family history closely, not only to determine whether there might be a genetic basis for the symptoms, but also to identify other people in the family who may carry the mutant gene, yet not exhibit symptoms of the disease.15 These individuals could benefit from genetic counseling and early monitoring for symptoms.
- What are the symptoms associated with ATTR-PN?
At the onset of the disease, people with ATTR-PN experience neurologic changes, including:2
- Numbness in the feet
- Decreased temperature sensation
- Pin-prick feelings
ATTR-PN also affects the autonomic nervous system, which controls involuntary processes in the body. These symptoms may include:2
- Dizziness or fainting
- Bouts of constipation
- Abnormal heartbeat
- Unintentional weight loss
- How is ATTR-PN diagnosed?
ATTR-PN can be difficult to recognize and manage. Misdiagnosis is common and definitive diagnosis can be delayed for years, postponing adequate treatment and genetic counseling, and leading to possible irreversible damage.9,10
Red flag symptoms suggesting an ATTR-PN diagnosis would include progressive nerve cell damage and one or more of the following13,16
- Signs usually associated with early autonomic dysfunction (eg incontinence, dry mouth)
- Severe chronic diarrhea, constipation, or alternating bouts of constipation and diarrhea
- Weight loss that cannot be explained
- Impaired kidney function
- Floaters or vitreous opacity
- Heart failure symptoms
- History of Bilateral Carpal tunnel syndrome
The disease is commonly mistaken for other forms of neuropathy, including chronic inflammatory demyelinating polyneuropathy, progressive diabetic neuropathy, and paraneoplastic syndrome, caused by the presence of a tumor.17
Family history should be investigated, and a thorough neurological examination should be performed, including small-fiber assessment, nerve conduction studies, electro- and echocardiograms, and laboratory evaluations.11
TTR genotyping and tissue biopsy, using Congo red staining, should be performed to confirm amyloid deposition.2
Individuals who are suspected of carrying the gene, but who do not yet show any symptoms of the disease, should be monitored closely.13 Physicians should perform the following tests regularly:2
- Neurological screening (which should, ideally, be done annually)
- Clinical evaluation of weight, autonomic and renal function
- Regular eye exams
- Testing for carpal tunnel syndrome and cardiac function
- What is ATTR-CM?
ATTR-CM is significantly under or misdiagnosed, making it difficult to characterize worldwide prevalence.3
In ATTR-CM, receiving a correct diagnosis has historically been difficult because disease awareness is low among health care professionals, and misdiagnosis is common because patients often present with symptoms similar to more common causes of heart failure.3
There are two sub-types of ATTR-CM: hereditary (hATTR), which is caused by a mutation in the transthyretin gene and can occur in people as early as their 50s and 60s;1,18,19 or the wild-type form (wtATTR) which is associated with aging, and is thought to be more common, usually affecting men after age 60.1
- What are the symptoms associated with ATTR-CM?
- Shortness of breath
- Fatigue
- Swelling of the ankles
Often the disease is diagnosed only after symptoms have become severe.18
- How is ATTR-CM diagnosed?
Awareness of ATTR-CM (transthyretin amyloid cardiomyopathy) is low within the physician community, and as a result, continues to be significantly underdiagnosed.3
Patients suspected of having ATTR-CM should be evaluated by echocardiography or cardiac magnetic resonance imaging.20 These tests are not typically used to confirm an ATTR-CM diagnosis, though they help your doctor understand more about your heart and if ATTR-CM may be considered as a cause of your symptoms.
Once ATTR-CM is suspected, your doctor can perform several tests to help diagnose the disease or identify whether you or a loved one are at risk.21
- Nuclear Scintigraphy: This noninvasive imaging test can be used to detect ATTR-CM. During the test, a small amount of a radiotracer is injected, and after waiting for one to three hours, images are taken using a gamma camera, a special camera that can read emissions from the radiotracer. These images can help your doctor understand if transthyretin (TTR) amyloid fibrils are present in your heart.
- Cardiac Biopsy: This procedure involves taking a few small samples of heart muscle tissue for examination. A cardiologist conducts the biopsy while you’re awake, using a local anesthetic. If amyloid fibrils are found in the removed tissue, the tissue is sent out to a lab to determine whether they are TTR amyloid fibrils or another type of cardiac amyloidosis. Biopsies from other parts of the body may also be taken, but they are less accurate in detecting ATTR-CM.
- Genetic Testing: Once ATTR-CM is diagnosed, genetic testing and counseling is recommended. Genetic testing can confirm or rule out the hereditary form of ATTR-CM (hATTR), which may have implications for not only you as the patient but your family members as well. Genetic tests typically use a blood or saliva sample.
Transthyretin Amyloidosis (ATTR) Resources
Area of Focus: Rare Disease
Transthyretin Amyloidosis(ATTR) is a focus of our Rare Disease Therapeutic Area.
Visit Our Rare Disease Site DetailsClinical Trials
We proudly partner with thousands of study sites and tens of thousands of trial participants around the world. It's these clinical trials that lead to life-changing medicines.
Go to Pfizer Clinical Trials Site DetailsReferences
1. Ruberg FL, Berk JL. Transthyretin (TTR) Cardiac Amyloidosis. Circulation. 2012;126(10):1286-1300.
2. Ando Y, Coelho T, Berk JL, et al. Guideline of Transthyretin-Related Hereditary Amyloidosis for Clinicians. Orphanet J of Rare Diseases. 2013;(8):31.
3. Rapezzi C, et al. Cardiac Amyloidosis: The Great Pretender. Heart Failure Reviews. 2015;(20):117-124.
4. Benson M, et al. Rate of Progression of Transthyretin Amyloidosis. Am J Cardiol. 2011;108(2):285-289.
5. Siddiqi OK, Ruberg FL. Cardiac Amyloidosis: An Update on Pathophysiology, diagnosis and treatment. Trends Cardiovasc Med. 2017;1050-1738.
6. Stewart M, Alvir J, Cicchetti M, et al. Characterizing the High Disease Burden of Transthyretin Amyloidosis for Patients and Caregivers. Neurol Ther. 2018;7(2):349-364.
7. Benson MD, Kincaid JC. The Molecular Biology and Clinical Features of Amyloid Neuropathy. Muscle Nerve. 2007;(36):411-423.
8. Hou X, Aguilar M-I, Small DH. Transthyretin and Familial Amyloidotic Polyneuropathy: Recent Progress in Understanding the Molecular Mechanism of Neurodegeneration. FEBS J. 2007;(274):1637-1650.
9. Shirota Y, Iwata A, Ishiura H, et al. A case of Atypical Amyloid Polyneuropathy with Predominant Upper-Limb Involvement with Diagnosis Unexpectedly Found at Lung Operation. Intern Med. 2010;(49):1627-1631.
10. Pareyson D. Diagnosis of Hereditary Neuropathies in Adult Patients. Neurology. 2003;(250):148-160
11. Planté-Bordeneuve V. Update in the Diagnosis and Management of Transthyretin Familial Amyloid Polyneuropathy. J Neurol. 2014;(26):1227-1233.
12. Schmidt H, Waddington Cruz M, Botteman MF, et al. Global Epidemiology of Transthyretin Familial Amyloid Polyneuropathy: A Systematic Review. Poster presented at the XV International Symposium on Amyloidosis, Jul 3-7, 2016, Uppsala, Sweden.
13. Sekijima Y, Yoshida K, Tokuda T, Ikeda S. Familial Transthyretin Amyloidosis. In: Pagon RA, Bird TD, Dolan CR, Stephens K, eds. GeneReviews [Internet]. Seattle, WA: University of Washington, Seattle; 1993-2009. http://www.ncbi.nlm.nih.gov/. Accessed April 27, 2016.
14. Planté-Bordeneuve V1, Said G. Familial Amyloid Polyneuropathy. Lancet Neurol. 2011;10(12):1086-97.
15. NIH Genetic and rare Diseases Information Center. Hereditary Amyloidosis. https://rarediseases.info.nih.gov/diseases/6611/hereditary-amyloidosis. Accessed February 10, 2020.
16. Conceição I, González-Duarte A, Obici L, et al. “Red-flag” Symptom Clusters in Transthyretin Familial Amyloid Polyneuropathy. J Peripher Nerv Syst. 2016;21(1):5-9.
17. Adams D, et al. Expert Consensus Recommendations to Improve Diagnosis of ATTR Amyloidosis with Polyneuropathy. J Neurol. 2020.
18. Rapezzi C, Quarta CC, Riva L, et al. Transthyretin Related Amyloidoses and the Heart: A Clinical Overview. Nat Rev Cardiol. 2010;(7):398-408.
19. Swiecicki PL, Zhen DB, Mauermann ML, et al. Hereditary ATTR Amyloidosis: A Single-Institution Experience with 266 Patients. Amyloid. 2015;22(2):123-131.
20. Brownrigg J, Lumley M, et al. Diagnostic Performance of Imaging Investigations in Detecting and Differentiating Cardiac Amyloidosis: A Systematic Review and Meta-Analysis. ESC Heart Fail. 2019;6(5):1041-1051.
21. Nativi-Nicolau J, Maurer MS. Amyloidosis Cardiomyopathy: Update in the Diagnosis and Treatment of the Most Common Types. Curr Opin Cardiol. 2018;33(5):571-579.