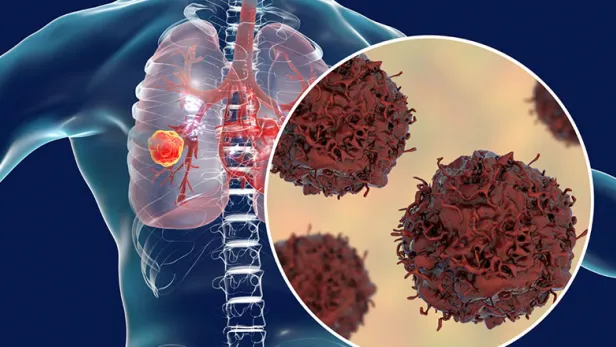
What Is Lung Cancer?
Lung cancer happens when cells in the lung grow out of control and form a tumor.5 Lung cancer always starts in the lung. Typically, it takes root in the cells lining the bronchi (the large air passages that lead from the trachea, or windpipe, to the lungs), the bronchioles (small branches of air tubes in the lungs), or alveoli (small air sacs where the lungs and the blood exchange oxygen).1
Prevalence of Lung Cancer
Worldwide, lung cancer is the top cause of cancer deaths and the most diagnosed cancer.2 In 2025, an estimated 226,650 new cases of lung cancer will be diagnosed in the United States and about 124,730 people will die from it.3 However, the rate of new annual lung cancer diagnoses in the U.S. has been declining. In 2021, there were 49.1 new cases for every 100,000 Americans, a drop from 62.9 new cases a decade earlier.4
Causes and Risk Factors
What Causes Lung Cancer?
Smoking cigarettes is the leading cause of lung cancer, but the disease can occur in people who have never smoked.6
The exact causes of lung cancer aren't known, but many factors can increase your risk. The clearest connection is between smoking and lung cancer. An estimated 85 percent of lung cancer deaths in 2025 are expected to be caused by smoking, and others attributed to secondhand smoke. Although lung cancer can occur in people who never smoked, it is less common.7

Lung Cancer and Genetics
A build-up of genetic changes in critical genes can lead to lung cancer.6 This can happen when changes occur in the genes that support cell growth, division, and survival (oncogenes) or in the genes that dictate cell division and death (tumor suppressor genes).7
In non-small cell lung cancer cases, for example:8
- Around 5 percent of NSCLC that occur in non-smokers result from mutations in the ALK gene.
- KRAS mutations are associated with about 20-25 percent of NSCLC cases cancers that develop in smokers and former smokers.
- Between 10-20 percent of NSCLC cells have high amounts of the EGFR protein on their surface, which helps them grow. These cases may be related to changes in the EGFR gene, which occurs more commonly among people who do not smoke, those who were assigned female at birth, and people of Asian descent.
- Around 1-2 percent of NSCLCs show changes to the ROS1 gene.
- In about 5 percent of cases, there are changes to the BRAF gene.
Patients typically acquire the genetic changes related to lung cancer during life. Experts have documented lifestyle and environmental factors that expose individuals to compounds that can cause cancer and increase the risk of genetic mutations, like cigarette smoke and air pollution.6 But the root causes of some changes remain unclear.7
Inherited genetic changes—which come from a person’s parents—can increase the risk of lung cancer, but inherited mutations are not associated with many lung cancer cases.7 Moreover, the increased risk may stem from shared environmental risk factors rather than inherited genetic changes.6
Lung Cancer Risk Factors
Not everyone who develops lung cancer smokes, and not everyone who smokes develops lung cancer. Lung cancer in nonsmokers and smokers may result from a combination of risk factors.7 Other risk factors for lung cancer include:10
- Asbestos. This material was often used as insulation in buildings, and people may be exposed through their jobs.
- Radon. Some rocks and soil release this odorless gas. While this is unlikely to be dangerous outdoors, homes and buildings can have high radon levels, especially in the basement.
- Air pollution. People exposed to outdoor air pollution from sources such as diesel engine exhaust may have a slightly higher risk for lung cancer.
Lung Cancer Prevention
Not smoking is the best way to prevent lung cancer. Avoiding secondhand smoke is also key to prevention.11
Environmental exposures through work or in the home can increase the risk of developing cancer.10 Wearing appropriate protective gear and following recommended work and safety procedures when working with asbestos or other cancer-causing agents can help reduce the risk of developing NSCLC.12 A radon detector can let you know when high levels of radon are present, and then you can take steps to reduce radon leaks.10,13
Metastatic Lung Cancer
Cancer can spread beyond the original tumor when the tumor sheds cancer cells. These cells enter the bloodstream or lymph nodes, where they can then spread to other parts of the body.14
Cancer is named by the original location of the tumor. If lung cancer spreads to another area of the body, it is called metastatic lung cancer.15
Lung cancer most often spreads to:16
- Nearby lymph nodes or other parts of the lung and chest
- Brain
- Bones
- Liver
- Adrenal glands
Other types of cancer can also spread to the lungs.17 Those cancers are still named after the original site of the tumor. For example, breast cancer that spreads to the lungs is called metastatic breast cancer.11 Cancers that most commonly spread to the lungs include:18
- Breast
- Colorectal
- Head and neck
- Kidney
- Testicular
- Uterine
- Lymphoma
Types of Lung Cancer
The two main types of lung cancer are non-small cell (NSCLC) and small cell (SCLC), with NSCLC being more prevalent than SCLC.1
NSCLC is the most common type of lung cancer, accounting for 80% to 85% of all lung cancer cases.1 The three main subtypes of NSCLC are:
- Adenocarcinoma. The most common subtype, adenocarcinoma, forms in the cells that line the surface of the lungs, which are responsible for making mucus. Some adenocarcinomas show changes in certain genes, such as the KRAS gene and the ALK gene.1,8 This type of lung cancer is typically slower growing compared to other types of lung cancer.9
- Squamous cell carcinoma. Another common subtype, squamous cell carcinoma starts in the flat cells that line the inside of the airways in the lungs, called squamous cells. This kind of lung cancer is more likely to be associated with smoking.1
- Large cell (undifferentiated) carcinoma. This subtype can appear in any part of the lung and can grow and spread quickly, making it more difficult to treat. Large cell neuroendocrine carcinoma (LCNEC) is a fast-growing subtype of large cell carcinoma that is similar to SCLC.1
SCLC affects about 10 to 20 percent of people with lung cancer.1,17 This cancer begins in the neuroendocrine, or hormone-producing, cells of the lungs.17 SCLC tends to spread quickly; for many people, the cancer cells have already spread beyond the lungs by the time they are diagnosed.1
Lung Cancer Symptoms
Symptoms of Lung Cancer
Most lung cancers do not cause noticeable symptoms until they have spread, but some people with early lung cancer may notice symptoms.19
The most common symptoms of lung cancer include:19
- Shortness of breath
- Coughing up blood
- Persistent cough
- Feeling tired or weak
- Chest pain that may get worse with coughing, laughing, or deep breathing
- Unexplained weight loss
- Loss of appetite
- Infections, such as pneumonia, that don't get better or come back
- Hoarseness

Lung Cancer–Related Syndromes
Lung cancer can sometimes lead to collections of symptoms considered syndromes, including:19
- Horner syndrome
More often associated with NSCLC, Horner syndrome is characterized by tumors that affect the upper part of the lung, called Pancoast tumors. Pancoast tumors can affect nerves around the eyes and face, causing eyelid droop, pupil constriction, and other facial symptoms.
- Superior vena cava syndrome
The superior vena cava is a large vein that carries blood to the heart from the head and arms, passing lymph nodes in the chest and the upper part of the right lung. Sometimes, tumors in this area can put pressure on this vein, causing swelling in the face, neck, arms, or chest. You may also feel dizzy or have headaches. This syndrome may develop gradually, but in some cases it can become life-threatening and should be treated immediately.
- Paraneoplastic syndromes
These syndromes are most often associated with SCLC but can occur with any type of lung cancer. Paraneoplastic endocrine syndrome occurs when hormone-like substances produced by the cancer cells enter the bloodstream. Although the cancer itself hasn't spread, these substances can cause symptoms throughout the body. Paraneoplastic neurologic syndrome occurs when the cancer cells cause the immune system to attack parts of the nervous system instead of the tumor. The symptoms from these syndromes are sometimes the first signs of lung cancer, but they aren't always suspected as lung cancer. Many symptoms of paraneoplastic syndromes are more likely to be caused by something else.
Lung Cancer Complications
Lung cancer can spread. Signs of metastasis can depend on where in the body the cancer has spread and may include:19
- Bone pain (such as pain in the back or hips)
- Nervous system changes (such as dizziness, headache, weakness, numbness of the limbs, or seizures)
- Jaundice (yellowing of the skin or eyes)
- Swelling in the lymph nodes

Biological Sex Differences in Lung Cancer
The types and number of lung cancer symptoms are similar at diagnosis for all sexes.20 However, the incidence of some lung cancers may vary by sex. People assigned female at birth tend to have higher rates of adenocarcinoma and lower rates of squamous cell carcinoma than people assigned male at birth. This may be due to differences between the groups in smoking habits.21
Diagnosis and Treatment
- Screening for Lung Cancer
Screening tests are designed to find illness before symptoms arise. People with lung cancer have a better chance of being treated successfully when the cancer is caught in earlier stages. However, regular chest X-rays as a screening tool for lung cancer haven't been proven to help most people live longer and are not recommended.22
Current lung cancer screening guidelines recommend yearly low-dose computed tomography (LDCT) scans for people who meet all the following three criteria:23
- Are 50 to 80 years old
- Currently smoke or used to smoke
- Have a 20 pack-year or more smoking history (a pack-year is the number of packs of cigarettes smoked per day multiplied by the number of years of smoking; for example, a person could have a 20 pack-year history by smoking one pack a day for 20 years or by smoking two packs a day for 10 years)
- Diagnostic Tests for Lung Cancer
Although some lung cancers may be found through screening tests, most are found because the cancer has caused symptoms. While evaluating for cancer, your doctor will perform a physical exam and ask about your history.8
Different imaging tests can help doctors look for cancer, track its spread, and evaluate a treatment’s progress. A doctor will decide which tests are most appropriate. Common lung cancer tests include:8
- CT scan
- Positron emission tomography, or PET, scan
- Magnetic resonance imaging, or MRI, scan
- Bone scan
To diagnose lung cancer, doctors collect a tissue, fluid, or mucus sample from the lung for evaluation. This is often done with a needle biopsy. During a needle biopsy, doctors use a hollow needle to take cells or pieces of tissue from a suspicious area to be examined under a microscope and sometimes to undergo molecular testing. In some cases, doctors perform a needle biopsy while a patient undergoes a bronchoscopy, a test used to look for tumors or blockages in the airways. Other ways to collect tissue samples include removing fluid from around the lungs (a procedure known as thoracentesis) or by using sputum samples that are coughed up. The specific testing or procedures needed for a biopsy may vary by patient.
A doctor may also perform blood tests, tests to see how well your lungs work, and tests to see whether the cancer has spread to the other areas.8
- Biomarker Testing for Lung Cancer
In biomarker testing, particularly for NSCLC, the doctor performs molecular testing of cell or tissue samples to look for specific genes or proteins that can provide information about the cancer cells, such as PD-L1, which is a protein that is expressed on the surface of certain cancer cells. Finding certain changes in the cancer cells can give doctors a better understanding of the genetic drivers of the disease and guide treatment options.8,24
- Stages of Lung Cancer
Lung cancer staging is based on the size and location of the tumor and whether the cancer cells have spread beyond the lungs to lymph nodes or distant organs. Based on test results and imaging, your doctor will determine the extent of disease that correlates to a stage.25
For NSCLC, stages range from stage 0 to stage 4 lung cancer. Higher stages correspond with more extensive disease. The stages of lung cancer are:25
- Stage 0 lung cancer. The tumor is found in the top layers of cells lining the airways but hasn't grown deeper into lung tissue or spread outside the lung.
- Stage 1 lung cancer. A small tumor has invaded deeper into the lung tissue but hasn't spread to nearby lymph nodes or other parts of the body.
- Stage 2 lung cancer. A larger tumor hasn't spread or a smaller tumor has spread to lymph nodes in the lung but not to distant organs.
- Stage 3 lung cancer. A larger tumor has spread to nearby lymph nodes but not to other parts of the body.
- Stage 4 lung cancer. The cancer has spread to the lining of the lungs or other areas of the body.
Doctors tend to stage SCLC using two categories:26
- Limited stage: The cancer is in one part of a patient's chest and potentially treatable with a single radiation field.
- Extensive stage: The cancer has spread widely throughout the lung, to the other lung, or to other areas of a patient’s body.
Lung Cancer Treatment
People diagnosed with lung cancer have a wide range of treatment options available. In addition to the options listed below, clinical trials of newer treatments may also be a good option for some people. If you’re interested in learning more about clinical trials available to you, talk with your doctor.27,28
NSCLC and SCLC have different treatment approaches. Many specialists—including thoracic surgeons, medical oncologists, radiation oncologists, and other healthcare professionals—work together to treat and manage the disease.27,28
A treatment plan considers the type, stage, and location of the cancer, along with results of biomarker testing, side effects, individual preferences, and your overall health and ability to tolerate treatment. A treatment plan may include a combination of different therapies.27,28
Surgery aims to remove the tumor completely. This may also include some lymph nodes if the medical team thinks that they might contain cancer cells. The surgeon also removes some additional tissue around the tumor for testing, sometimes including lymph nodes. This is to make sure that the surgeon has removed all the cancer cells.27,29
Surgery is not often used to treat SCLC and is usually reserved for a few cases of limited stage cancer.28 The different types of surgical procedures, particularly for NSCLC, include:27,29
- Pneumonectomy. The entire lung is removed.
- Lobectomy. One lobe of the lung is removed. This surgery is usually the preferred surgical approach when it's possible.
- Sleeve resection. Removal of a portion of the airway.
- Wedge resection. When removing an entire lobe isn’t possible, the tumor and some surrounding lung tissue are removed. This is often done in individuals who don't have enough lung function to withstand the removal of a full lobe.29
Surgery for lung cancer carries risks similar to any major surgery, including blood clots, infection, and bleeding. Pneumonia is also possible. It can take weeks or months to recover from surgery, depending on the complexity of your procedure.29
Chemotherapy involves intravenous or oral cancer-fighting medications. For NSCLC, chemotherapy can be used before and after surgery, and it’s sometimes used to treat cancer that has spread beyond the lungs. If surgery isn’t an option for someone, chemo may be used in combination with radiation therapy as a main treatment.30 Chemotherapy with radiation therapy is the most common treatment for limited-stage SCLC.28
Patients can receive a combination of drugs that work for their specific cancer type.30 But chemotherapy drugs may affect healthy cells along with cancer cells and have the potential for a range of side effects. Common side effects include fatigue, loss of appetite, hair loss, nausea, vomiting, mouth sores, and higher risk for infection. These side effects usually go away once chemotherapy treatment is over.30
Radiation therapy is commonly used for NSCLC and uses high-energy X-rays or other particles to kill cancer cells. It may be the primary treatment for people who can't undergo surgery, sometimes along with chemotherapy. It may also be used before surgery to shrink a tumor, or after surgery to kill any remaining cancer cells.31 In SCLC, it may be used to treat cancer for people with limited disease and to alleviate symptoms and prevent the spread of cancer cells to other parts of the body, especially the brain, in people with extensive disease.28
This kind of therapy can cause skin irritation, nausea, vomiting, loss of appetite, and sometimes, hair loss where the radiation beam contacts the skin. Many side effects go away when treatment stops.31
Immunotherapy uses the body's own immune system to fight cancer. These treatments target certain immune system pathways to help the immune system slow or stop the growth of cancer cells.32
One type of immunotherapy commonly used to treat lung cancer is called immune checkpoint inhibitors. Certain proteins on immune cells act as switches that control when an immune response is turned on or off. Some cancer cells can use these “checkpoint” proteins to avoid a response from the immune system. Immune checkpoint inhibitors target these checkpoint proteins to treat some people with lung cancer. Available immunotherapy options include:33,34
- PD-1/PD-L1 inhibitors
- CTLA-4 inhibitors
- Bispecific T-cell engager (BiTE)
Immunotherapies are available to treat NSCLC and SCLC either alone or in combination with other therapies, including other immunotherapies or chemotherapy. The choice of treatment depends on many factors, including your type of cancer, stage, and health.26,28
These treatments are associated with side effects, such as fatigue, nausea, itching, and diarrhea. Other side effects related to the medication's effects on the immune system are possible.33,34
Targeted therapies are medications that work to directly target proteins that regulate cancer growth and spread. These therapies are chosen based on biomarker or molecular testing of tumor samples to understand the characteristics of the cancer.35 Targeted therapies currently available for NSCLC include:37
- Angiogenesis inhibitors
- KRAS inhibitors
- EGFR inhibitors
- ALK inhibitors
- ROS1 inhibitors
- BRAF inhibitors
- RET inhibitors
- MET inhibitors
- HER2-directed drugs
- TRK inhibitors
Living With Lung Cancer
Getting a cancer diagnosis can bring about a lot of emotions.38
Each type of treatment may have a different recovery journey, and some may have long-term side effects.38
Maintaining a healthy lifestyle, with moderate physical activity and healthy foods, can help overall health. If you haven't quit smoking, quitting now may still benefit you.38
You may consider support from family, friends, and professionals or support groups. Many resources are available to answer questions or connect you to supportive care.38
Lung Cancer Prognosis
The outlook and survival time for lung cancer vary by stage, type of cancer, and genetic characteristics of the cancer, as well as by patient age and overall health, along with many other factors.39
Relative survival rates offer some insight into an individual’s recovery by comparing the survival rates of people who have the same type and stage of cancer and the general population. For exmple, if a lung cancer patient’s five-year relative survival rate at diagnosis is 60 percent, the patient is 60 percent as likely to live five years after diagnosis as people who do not have the disease.39
People who are diagnosed now may have a better outlook than the current numbers show because newer treatment options steadily improve the approach to lung cancer treatment and the lung cancer survival rates.39
Five-year survival rates for NSCLC are estimated to be:39
- Overall: 28 percent
- Localized disease, showing no sign that the cancer has spread outside the lung: 65 percent
- Regional disease, in which the cancer has spread to nearby structures or lymph nodes outside the lung: 37 percent
- Distant disease, in which the cancer has spread to distant parts of the body: 9 percent
For SCLC, five-year survival rates are estimated to be:39
- Overall: 7 percent
- Localized disease: 30 percent
- Regional disease: 18 percent
- Distant disease: 3 percent
Global Impact of Lung Cancer

As the most commonly diagnosed cancer in the world, lung cancer cases reached nearly 2.5 million in 2022. It is the leading cause of cancer death worldwide.40
The global annual cost of cancer, including direct healthcare costs and disability, totals hundreds of billions of dollars and is expected to increase.42 In the United States, lung cancer cost an estimated $23.8 billion in 2020 alone.43
The United States and many countries in Europe experienced a tobacco epidemic early and have since seen declines in smoking and lung cancer. Other countries that experienced tobacco epidemics later are still experiencing increasing lung cancer rates.42
Frequently Asked Questions About Lung Cancer
- What is the lung cancer survival rate?
The overall five-year relative survival rate for NSCLC for all stages is 28 percent. The overall five-year relative survival rate for SCLC is 7 percent. However, these numbers do not fully reflect the advances made in lung cancer treatment within the past decade. Survival varies by type of disease, the molecular characteristics of the disease, age, overall health, and other factors.39
- What percentage of smokers get lung cancer?
Cigarette smoking is the main risk factor for lung cancer. Smokers are 15 to 30 times more likely than nonsmokers to develop lung cancer or die from lung cancer. Quitting smoking immediately starts to lower your risk for developing cancer.43
- How do I get screened for lung cancer?
Screening tests are designed to find illness before symptoms arise. People with lung cancer have a better chance of being treated successfully when the cancer is caught in earlier stages.22 If you’re 50 to 80 years old, currently smoke or used to smoke, and have a 20 pack-year or more smoking history, it’s recommended that you get annual screening.23
Although some lung cancers are found through screening tests, most are found because the cancer has caused symptoms. While evaluating for cancer, your doctor will perform a physical exam and ask about your history.8
Different imaging tests can help doctors look for cancer, track its spread, and evaluate a treatment’s progress. A doctor will decide which tests are most appropriate.8
- If I’m diagnosed with lung cancer, where do I begin?
People diagnosed with lung cancer have a wide range of treatment options available. Your doctor will work with you to determine which course of treatment is best for you.27,28
- Is lung cancer curable?
For most people, available treatments do not cure NSCLC or SCLC.27,28,44 But for some early-stage NSCLC, surgery may effectively offer a cure.24 Various factors impact lung cancer survival rates, including the type of lung cancer, the stage of the cancer, and the patient’s overall health.27,28
- Is lung cancer genetic?
People with a family history of lung cancer tend to be at slightly higher risk for developing the disease, but this may be based on shared risk factors rather than inherited genetic changes. Most lung cancers are caused by genetic changes that are acquired over a person’s life.6
Many lung cancers are linked to non-hereditary genetic changes in cellular DNA.6 The causes of these abnormalities are unclear because they are not inherited from relatives, but they may be associated with certain risk factors. For example, a mutation in the KRAS gene is present in about 20 percent to 25 percent of non–small cell lung cancers (NSCLCs). This gene change helps the cancer cells to grow and spread. These gene changes have been found to affect the disease and treatment options.8
About 5 percent of NSCLCs have a change in the ALK gene, which is more often seen in non-smokers and light smokers. Other examples include NSCLCs that have a rearrangement in the ROS1 gene, seen in 1-2 percent of cases, or changes in the BRAF gene, detected in about 5 percent of cases.8
Learn More About Lung Cancer
Find Pfizer clinical trials for lung cancer at PfizerClinicalTrials.com.
Explore lung cancer clinical trials at ClinicalTrials.gov.
Area of Focus: Oncology
Lung Cancer is a focus area for Pfizer Oncology. To learn more about how we’re accelerating breakthroughs to outdo cancer, visit the Oncology page.
Find resources for those living with cancer and their caregivers at This is Living with Cancer.
- References
- What is lung cancer? American Cancer Society. https://www.cancer.org/cancer/lung-cancer/about/what-is.html. Updated January 29, 2024. Accessed May 22, 2025.
- Lung cancer kills more people worldwide than other cancer types. American Cancer Society. https://www.cancer.org/research/acs-research-news/lung-cancer-kills-more-people-worldwide-than-other-cancers.html. Updated July 29,2024. Accessed May 27, 2025.
- Cancer facts & figures 2025. American Cancer Society. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2025/2025-cancer-facts-and-figures-acs.pdf. Updated 2025. Accessed May 22, 2025.
- Trends. Changes over time: Lung and bronchus. New Cancers, all ages, all races and ethnicities, male and female. Centers for Disease Control and Prevention. https://gis.cdc.gov/Cancer/USCS/#/Trends/. Accessed May 22, 2025.
- Lung cancer basics. Centers for Disease Control and Prevention. https://www.cdc.gov/lung-cancer/about/. Updated October 15, 2024. May 22, 2025.
- Lung cancer. MedlinePlus. https://medlineplus.gov/genetics/condition/lung-cancer/. Accessed May 22, 2025.
- What causes lung cancer? American Cancer Society. https://www.cancer.org/cancer/lung-cancer/causes-risks-prevention/what-causes.html. Updated January 29, 2024. Accessed May 22, 2025.
- Tests for lung cancer. American Cancer Society. https://www.cancer.org/cancer/lung-cancer/detection-diagnosis-staging/how-diagnosed.html. Last updated January 29, 2024. Accessed May 22, 2025.
- Lung adenocarcinoma. Lungevity Foundation. https://www.lungevity.org/lung-cancer-basics/types-of-lung-cancer/lung-adenocarcinoma. Updated February 10, 2024. Accessed May 22, 2025.
- Lung cancer Risk factors and prevention. American Cancer Society. https://www.cancer.net/cancer-types/lung-cancer-non-small-cell/risk-factors-and-prevention. Updated January 29, 2024. Accessed May 22, 2025.
- Lung cancer prevention (PDQ®)—patient version. National Cancer Institute. https://www.cancer.gov/types/lung/patient/lung-prevention-pdq. Updated July 26, 2024. Accessed May 22, 2025.
- Asbestos and cancer risk. American Cancer Society. https://www.cancer.org/cancer/risk-prevention/chemicals/asbestos.html. Updated October 3, 2023. Accessed May 27, 2025.
- Radon and cancer. American Cancer Society. https://www.cancer.org/cancer/risk-prevention/radiation-exposure/radon.html. Updated November 1, 2022. Accessed May 22, 2025.
- How does cancer spread? American Cancer Society. https://www.cancer.org/cancer/managing-cancer/advanced-cancer/how-does-cancer-spread.html. Updated July 9, 2024. Accessed May 27, 2025.
- What are advanced and metastatic cancer. American Cancer Society. https://www.cancer.org/treatment/understanding-your-diagnosis/advanced-cancer/what-is.html. Updated July 9, 2024. Accessed May 22, 2025.
- About advanced lung cancer. Cancer Research UK. https://www.cancerresearchuk.org/about-cancer/lung-cancer/advanced/about. Last reviewed March 20, 2023. Accessed May 22, 2025.
- Types of lung cancer. Cancer Research UK. https://www.cancerresearchuk.org/about-cancer/lung-cancer/stages-types-grades/types#:~:text=cell%20lung%20cancer.-,Small%20cell%20lung%20cancer%20(SCLC),neuroendocrine%20cells%20of%20the%20lung. Updated December 30, 2022. Accessed May 22, 2025.
- Lung metastases. American Cancer Society. https://www.cancer.org/treatment/understanding-your-diagnosis/advanced-cancer/lung-metastases.html. Updated September 10, 2020. Accessed May 22, 2025.
- Signs and Symptoms of Lung Cancer. American Cancer Society. https://www.cancer.org/cancer/lung-cancer/detection-diagnosis-staging/signs-symptoms.html. Last revised January 29, 2024. Accessed May 22, 2025.
- Ruano-Ravina A, Provencio M, Calvo de Juan V, et al. Are there differences by sex in lung cancer characteristics at diagnosis? -a nationwide study. Transl Lung Cancer Res. 2021;10(10):3902-3911. doi:10.21037/tlcr-21-559
- Stabellini N, Bruno DS, Dmukauskas M, et al. Sex Differences in Lung Cancer Treatment and Outcomes at a Large Hybrid Academic-Community Practice. JTO Clin Res Rep. 2022;3(4):100307. Published 2022 Mar 9. doi:10.1016/j.jtocrr.2022.100307
- Can lung cancer be found early? American Cancer Society. https://www.cancer.org/cancer/lung-cancer/detection-diagnosis-staging/detection.html. Updated January 29, 2024. Accessed May 22, 2025.
- Lung Cancer Screening Guidelines. American Cancer Society. https://www.cancer.org/health-care-professionals/american-cancer-society-prevention-early-detection-guidelines/lung-cancer-screening-guidelines.html. Accessed May 22, 2025.
- Biomarker testing for cancer treatment. National Cancer Institute. https://www.cancer.gov/about-cancer/treatment/types/biomarker-testing-cancer-treatment. Updated December 14, 2021. Accessed May 22, 2025.
- Non-small cell lung cancer stages. American Cancer Society. https://www.cancer.net/cancer-types/lung-cancer-non-small-cell/stages. Updated January 29, 2024. Accessed May 22, 2025.
- Small cell lung cancer stages. American Cancer Society. https://www.cancer.net/cancer-types/lung-cancer-small-cell/stages. Updated January 29, 2024. Accessed May 22, 2025.
- Treatment choices for non-small cell lung cancer, by stage. American Cancer Society. https://www.cancer.net/cancer-types/lung-cancer-non-small-cell/types-treatment. Updated October 29, 2024. Accessed May 22, 2025.
- Treatment choices for small cell lung cancer, by stage. American Cancer Society. https://www.cancer.net/cancer-types/lung-cancer-small-cell/types-treatment. Updated December 6, 2024. Accessed May 22, 2025.
- Surgery for non-small cell lung cancer. American Cancer Society. https://www.cancer.org/cancer/lung-cancer/treating-non-small-cell/surgery.html. Updated January 29, 2024. Accessed May 22, 2025.
- Chemotherapy for non-small cell lung cancer. American Cancer Society. https://www.cancer.org/cancer/lung-cancer/treating-non-small-cell/chemotherapy.html. Updated January 29, 2024. Accessed May 22, 2025.
- Radiation therapy for non-small cell lung cancer. American Cancer Society. https://www.cancer.org/cancer/lung-cancer/treating-non-small-cell/radiation-therapy.html. Updated January 29, 2024. Accessed May 22, 2025.
- How immunotherapy is used to treat cancer. American Cancer Society. https://www.cancer.org/cancer/managing-cancer/treatment-types/immunotherapy/what-is-immunotherapy.html. Updated December 27, 2019. Accessed May 22, 2025.
- Immunotherapy for non-small cell lung cancer. American Cancer Society. https://www.cancer.org/cancer/lung-cancer/treating-non-small-cell/immunotherapy.html. Updated September 23, 2024. Accessed May 22, 2025.
- Immunotherapy for small cell lung cancer. American Cancer Society. https://www.cancer.org/cancer/lung-cancer/treating-small-cell/immunotherapy.html. Updated December 26, 2024. Accessed May 22, 2025.
- Targeted therapy to treat cancer. National Cancer Institute. https://www.cancer.gov/about-cancer/treatment/types/targeted-therapies. Updated May 31, 2022. Accessed May 22, 2025.
- Non-small cell lung cancer treatment (PDQ)—patient version. National Cancer Institute. https://www.cancer.gov/types/lung/patient/non-small-cell-lung-treatment-pdq. Updated October 11, 2024. Accessed May 22, 2025.
- Targeted drug therapy for non-small cell lung cancer. American Cancer Society. https://www.cancer.org/cancer/types/lung-cancer/treating-non-small-cell/targeted-therapies.html. Updated December 6, 2024. Accessed May 22, 2025.
- What to expect from your lung cancer journey. American Lung Association. https://www.lung.org/lung-health-diseases/lung-disease-lookup/lung-cancer/living-with-lung-cancer/what-to-expect. Updated September 25, 2024. Accessed May 22, 2025.
- Lung cancer survival rates. American Cancer Society. https://www.cancer.org/cancer/lung-cancer/detection-diagnosis-staging/survival-rates.html. Updated January 29, 2025. Accessed May 22, 2025.
- Global Cancer Facts & Figures Fifth Edition. American Cancer Society. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/global-cancer-facts-and-figures/global-cancer-facts-and-figures-2024.pdf. Published 2024. Accessed May 22, 2025.
- Global Cancer Facts & Figures Fourth Edition. American Cancer Society. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/global-cancer-facts-and-figures/global-cancer-facts-and-figures-4th-edition.pdf. Published 2018. Accessed May 22, 2025.
- Lung cancer trends brief. American Lung Association. https://www.lung.org/research/trends-in-lung-disease/lung-cancer-trends-brief/lung-cancer-additional-measures. Accessed May 22, 2025.
- Lung cancer risk factors. Centers for Disease Control and Prevention. https://www.cdc.gov/cancer/lung/basic_info/risk_factors.htm. Updated October 15, 2024. Accessed May 22, 2025.
- Small cell lung cancer treatment (PDQ®)—patient version. National Cancer Institute. https://www.cancer.gov/types/lung/patient/small-cell-lung-treatment-pdq. Updated November 1, 2024. Accessed May 22, 2025.
The information contained on this page is provided for your general information only. It is not intended as a substitute for seeking medical advice from a healthcare provider. Pfizer is not in the business of providing medical advice and does not engage in the practice of medicine. Pfizer under no circumstances recommends particular treatments for specific individuals and in all cases recommends consulting a physician or healthcare center before pursuing any course of treatment.
Related Articles
Lung Cancer: The Facts
If someone were to ask you what the leading cause of cancer-related death is in the US, you might guess colon cancer, breast cancer, or prostate cancer. The correct answer is actually lung cancer. It’s also the second most diagnosed cancer in the US in both men and women. Most people diagnosed...
How Biomarkers Can Help With Lung Cancer Treatment
Lung cancer is the most common cause of cancer death in both men and women. In fact, it is estimated that nearly 230,000 lung cancer cases will be diagnosed in the United States in 2020. Of those cases, 80-85% of lung cancer is non-small cell lung cancer (NSCLC).1 The treatment of patients with...