Viral vs. Bacterial Pneumonia: Understanding the Difference

Having pneumonia can be frightening because this illness directly impacts one vital function — our breathing. For those who are at high risk of getting pneumonia and the complications that may accompany it, it is very important to make an accurate diagnosis.
According to the World Health Organization’s most current statistical data, pneumonia is one of the leading causes of death in children — responsible for 18% of all deaths in children under age five. Many of these outcomes can be prevented with global measures that increase access to immunizations, adequate pre and post-natal care for mother and baby, sufficient nutrition, and clean water.1
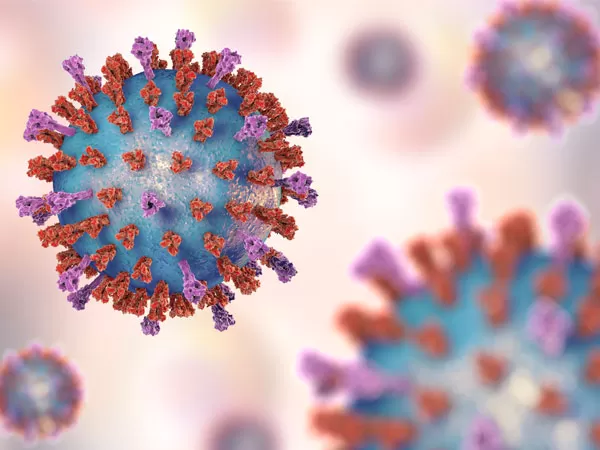
The two most common causes of pneumonia are from viral pathogens or bacterial pathogens. Some types of bacterial pneumonia can be prevented with vaccines, such as the aggressive bacteria Strep. Pneumoniae, prevented with the pneumococcal vaccine. Despite increasing vaccine availability globally, the persistence of Strep pneumonia infections remains. At the same time, vaccine utilization remains stagnant.
In the most recent 2020 textbook update from Biomedical Science, scientists state, “Diagnosis [of pneumonia] still remains challenging for medical providers. Because bacterial pneumonia can be treated with antibiotics, it is important to be able to differentiate between viral and bacterial pneumonia.2
What are the main differences between bacterial and viral pneumonia?
Common symptoms of pneumonia include3
- cough
- fever
- difficulty breathing
- increased breathing rate
When a patient presents with these symptoms, the next step is to examine the lungs with a stethoscope. With pneumonia, decreased breath sounds, wheezing, or crackles on listening to the lungs, are all indications that can help point towards a diagnosis. The next step is to order a radiograph or X-ray if pneumonia is suspected.
The radiograph still remains the reference standard for a medical diagnosis of pneumonia, and also helps to differentiate between bacterial and viral pneumonia. However, a combination of clinical symptoms, exam findings, and imaging is the best way to uncover the most likely culprit.3,4
Classic Viral Pneumonia
Often viral cases of pneumonia begin as congestion and cough with or without fever in the first few days. When a doctor listens to the lungs and finds breathing sounds are not clear on either side of the chest, a viral cause over bacterial is even more highly suspected. Viruses affect both sides of the lungs by producing a more homogeneous inflammatory reaction that causes increased cellular debris and mucus where previously open lung pockets were present. An X-ray is likely to demonstrate a more “diffuse” involvement of the lungs.3,4
Classic Bacterial Pneumonia
When a provider hears lung sounds that seem normal on one side but absent on the other, bacterial pneumonia is more likely. Bacteria tend to aggressively attack one lobe or section of the lungs causing a specific area of inflammation to take over the cells that were filled with air. An X-ray will show one white condensed area or opacity with the other areas of the lung visualized as having normal air exchange.5
While the process of combining the presence of respiratory symptoms with an abnormal exam and X-ray helps to delineate the cause of pneumonia, the only gold standard test to confirm the presence of a specific pathogen is a culture (a sample of respiratory mucous secretions or blood that is analyzed in the lab for the presence of a virus or bacteria). If a culture grows one particular microorganism, you know the exact cause.
Critical Role of Pneumococcal Vaccine in Preventing Pneumonia
In children aged three months to four years, the most common type of bacterial pneumonia is Strep. pneumoniae. In children greater than age four, it remains in the top three most common types. The pneumococcal vaccine series, started at two months of age, significantly reduces the rates of bacterial pneumonia from Strep. Pneumoniae. The vaccine is usually administered during wellness or prevention visits and cannot be given to a child with a fever. This emphasizes the need for healthcare access globally.6
With global vaccination rates currently plateauing, the challenges of diagnosing and treating community acquired pneumonia are even more pertinent for prevention of severe respiratory illness. Vaccine uptake challenges can be overcome with global measures to increase the access and use of vaccines. Addressing vaccine use and providing education about common pneumonia symptoms can aid in early diagnosis of pneumonia and lower the rate of severe respiratory illness and prolonged hospitalization.
References
World Health Organization Health Topics. Immunization, Vaccines and Biologicals: National programs and systems on improving vaccination demand and addressing hesitancy. 17 June 2020 update.
Popovsky EY, Florin TA. Community-Acquired Pneumonia in Childhood. Reference Module in Biomedical Sciences. 2020;B978-0-08-102723-3.00013-5. doi:10.1016/B978-0-08-102723-3.00013-5
- Shah SN, Bachur RG, Simel DL, Neuman MI. Does This Child Have Pneumonia?: The Rational Clinical Examination Systematic Review [published correction appears in JAMA. 2017 Oct 3;318(13):1284].JAMA. 2017;318(5):462-471. doi:10.1001/jama.2017.9039
Hunton R. Updated concepts in the diagnosis and management of community-acquired pneumonia. JAAPA. 2019;32(10):18-23. doi:10.1097/01.JAA.0000580528.33851.0c
- Reynolds JH, McDonald G, Alton H, Gordon SB. Pneumonia in the immunocompetent patient.Br J Radiol. 2010;83(996):998-1009. doi:10.1259/bjr/31200593
Alicino C, Paganino C, Orsi A, et al. The impact of 10-valent and 13-valent pneumococcal conjugate vaccines on hospitalization for pneumonia in children: A systematic review and meta-analysis. Vaccine. 2017;35(43):5776-5785. doi:10.1016/j.vaccine.2017.09.005
![]()
![]()