Customizing Viral Vectors to Further Gene Therapy Innovation
It seems strange to think that a harmless virus could be the key to treating an illness. But an innovative and transformative medicine called gene therapy uses non-disease-causing viruses to deliver a healthy copy of a gene that aims to treat the underlying cause of a disease. These viruses are used as vectors or vehicles that deliver genetic materials to specific cells.1
“As this flourishing field expands, scientists are engineering viral vectors that are more precisely able to deliver therapeutic genes to targeted cells and tissues,” says Sury Somanathan, Head of AAV Gene Therapy at Pfizer's Kendall Square site. “Hopefully, these targeted gene therapies will be available in the future for a wide range of diseases.”
How Does Gene Therapy Work?
Gene therapy is an emerging area of science and medicine exploring the use of genes to treat certain diseases. Genes make proteins, and variations or mutations in those proteins can cause disease. Gene therapy delivers a healthy copy of a gene into a cell to replace or inactivate a damaged gene or to augment expression of missing proteins.1,2
Two types of gene therapies are used: ex vivo, which means “outside the body” and involves altering cells in the lab, and in vivo, an approach that sends gene-editing tools or gene modulators to target the affected tissue.2
Single-gene disorders are ideal for gene therapy because they involve a disease-causing variation (mutation) in only one gene. This specific gene is known, establishing a clear target.2 Science shows promising results in the ability to repair single, disease-causing genes to treat blood disorders and degenerative muscle and eye diseases. Since 2016, several gene therapy treatments have received FDA approval and more clinical trials are expected to test the potential of gene therapy to treat additional conditions.2
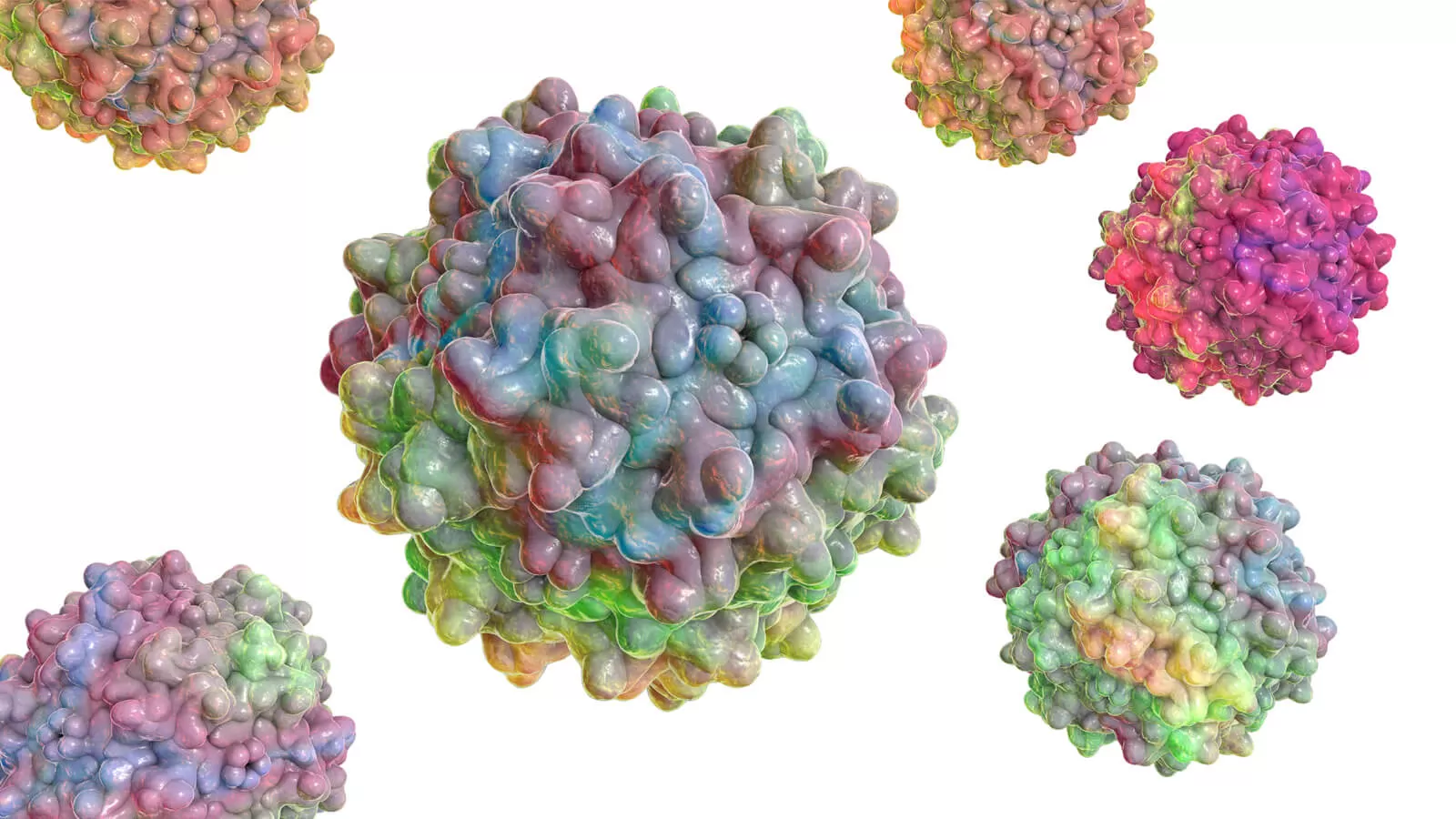
For gene therapy to work, scientists need ways to deliver genes into specific cells. Vectors use the shell of the virus, called the capsid, to deliver a healthy copy of a gene into a cell. But merely delivering a gene into a cell doesn't make it function properly; the gene needs to survive in the cell and be turned on. Only then can a vector provide the benefits of the treatment.3
Viruses such as adeno-associated viruses (AAVs) are commonly used as vectors for gene therapy given their ability to deliver genes to non-dividing cells where the gene has a long-term therapeutic impact. Different types of AAVs are known to target different cells, making them an ideal transporter of genetic material to desired locations within the body, providing a customized treatment.4,5
“Scientists are developing a toolbox of AAV vectors with the capability of targeting specific tissues in the body,” says Stephen Kagan, Global Medical Lead, Gene Therapy Platform and Cross Portfolio at Pfizer. “The addition of regulatory elements can then further help to direct expression at the tissue of interest, like at the liver or the muscle, for example.”
Challenges in Gene Therapy Methods
Viral vectors are designed to deliver genes to the appropriate cells,3 but developing this innovative area is quite complex. Our bodies have evolved to naturally fight off viruses, not welcome them.
A small percentage of patients who are naturally exposed to AAVs already have antibodies primed and ready to attack and inactivate viruses. In these patients, the vector isn't always able to successfully deliver the gene of interest into the target cell. However, recombinant AAV vectors remain the most used delivery vehicles for in vivo gene therapy.2,4,5
"Being able to engineer around our bodies' natural ability to combat viruses is our biggest challenge," says Somanathan.
This engineering process starts with the vector's outer protein shell, called a capsid. In an AAV vector, the healthy copy of the gene is encased inside the capsid. Within the vector, it replaces the AAV viral genetic material.4
Upon entry into a cell, the virus breaks down and delivers the DNA into the cell nucleus. Within the nucleus the gene is "turned on" or transcribed into RNA like messenger RNA (mRNA). The mRNA starts making therapeutic proteins while gene-editing systems that are introduced into cells as a virus or part of an RNA-protein complex can change target genes.1,2
For gene therapy to work, the AAV vector needs to reach the cells without alerting the patient’s immune system. Capsids are critical to this success and scientists are working hard to develop optimal stealth capsids to target the desired cell type while reducing host immune system activation.4
Rational Design for Viral Vector Engineering
Rational design is one of the methods Pfizer uses to develop capsids. Rather than approaching the challenges with a trial-and-error process, rational design uses high-tech tools to test possible viral capsids.5 For AAV vector engineering, rational design applies knowledge of a virus’ structure plus how the virus interacts with the external environment. The engineering process then uses modeling technology to test solutions for evading the immune response.5
Pfizer scientists aim to engineer capsids and design vectors to deliver genetic material and treatments with precision. They are identifying novel capsids, optimal routes of administration, and ways to modulate the immune response to create effective gene therapies, Somanathan says. Pfizer is evaluating engineered AAVs that target select disease-causing tissues.
"Pfizer's approach is to use a combination of capsid engineering and vector design with optimal regulatory elements to restrict expression to target organs to treat various genetic disorders," Somanathan says. "In the end, we aim to create a battery of precision medicines to treat a variety of rare genetic disorders. And in the future, there is hope that gene therapy could even be a solution for more common diseases, as well.”
So far, only a handful of gene therapies are approved in the United States and Europe.2,5 However, the U.S. Food and Drug Administration predicts the approval of 10 to 20 new cell and gene therapy products per year by 2025.6
Gene therapy holds promise as a targeted, precise form of treatment, but there is still much research underway. With increasing knowledge and new advances in delivery methods, gene therapy may be available to more people to treat disorders that currently have limited treatment options.2,5