Riding the Wave to Non-Invasive NASH Diagnosis
As early as ancient Greece, doctors used a method called palpation to diagnose illness, pressing their hands on a patient’s abdomen to assess the firmness of diseased tissues and organs.
This ancient practice is now getting a 21st-century upgrade. Scientists are working to develop advanced techniques to measure the stiffness of the liver to better diagnose NASH or non-alcoholic steatohepatitis, a serious, progressive form of NAFLD, or non-alcoholic fatty liver disease.
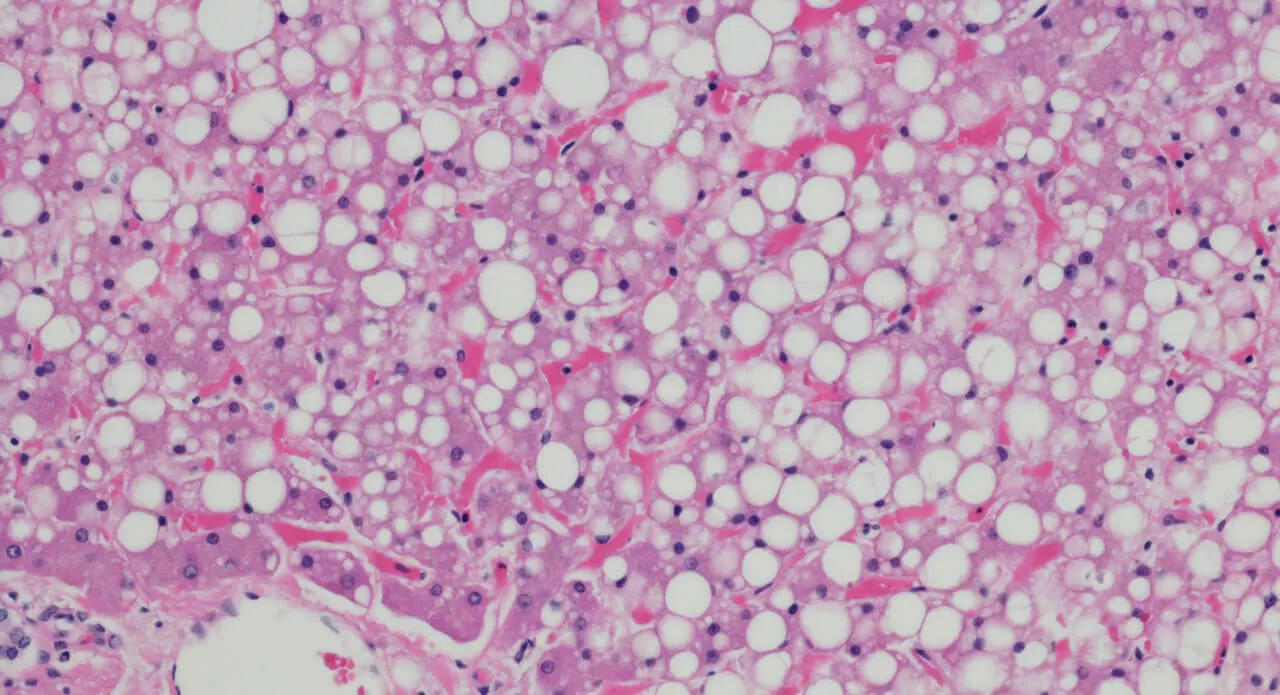
NASH is caused by the accumulation of fat in the liver, inflammation, cell damage, and eventually in some patients with fibrosis, scarring of tissue that leads to increased liver stiffness. Often called a “silent disease,” NASH can develop over years before a patient feels sick. But once it’s advanced, there are few treatments available, and patients may require a liver transplant. While experts don’t know the exact cause of NASH, it is linked to metabolic syndrome, diabetes and obesity.
Virtual palpation
Currently, the only way to definitively diagnose NASH is through a liver biopsy, which is invasive and painful for people. Another limitation of using liver biopsy is that it only captures a very small tissue sample and does not provide a complete picture of organ damage. But Pfizer Digital Medicine and Translational Imaging scientists, along with colleagues in the Internal Medicine Research Unit, are currently collaborating with leading academic researchers at the University of Wisconsin and University of California at San Diego to develop and test 3D elastography tools — tracking sound waves sent through the liver — to measure mechanical properties of the entire organ and ultimately diagnose the disease.
“By being able to come up with non-invasive imaging techniques, we hope to ultimately help patients avoid having to undergo a biopsy,” says James Goodman, a Senior Director in Pfizer’s Digital Medicine and Translational Imaging (DMTI) group. “These important techniques will also help us more easily identify subjects to enroll in clinical studies, as well as potentially serve as a metric by which we can assess the efficacy of new compounds,” he adds.
“Putting a number on it”
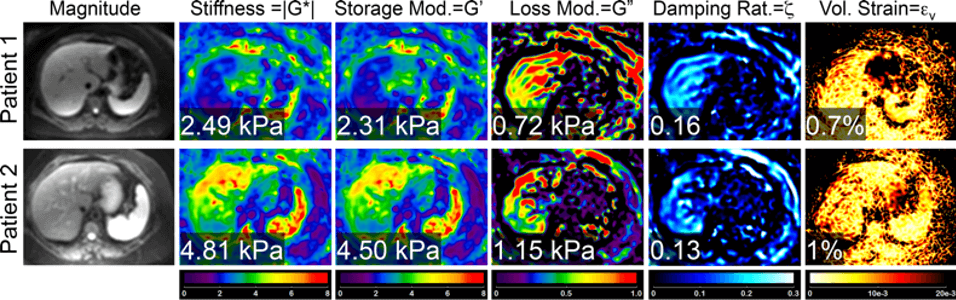
The Pfizer team is currently collaborating with Dr. Scott Reeder at the University of Wisconsin and Dr. Claude Sirlin at the University of California at San Diego to develop and test the robustness of these 3D elastography techniques, which will enable measurement of multiple factors that describe in detail the overall mechanical properties of the liver. Existing methods measure the sound wave propagation in one direction, enabling an assessment of stiffness to which fibrosis (or scarring), fat and inflammation can all contribute. While this is valuable, this technique lacks sensitivity to early phases of liver disease and it is still difficult to uniquely interpret the underlying cause of the stiffness measured in the traditional way. “By tracking the sound wave in multiple dimensions, instead of in just one dimension, we’re able to pull out a number of different mechanical properties which appear to be related to the inflammatory aspect of the disease,” says Goodman. “Understanding the inflammatory state of the liver is particularly important in staging the disease in its early phases and is currently only accessible by biopsy.”
The technique works by placing an acoustic driver — the size of a ping pong paddle — on the patient’s abdomen to send gentle vibrations through the liver. The patient is placed inside an MRI scanner, where the speed at which the wave moves through the liver in three dimensions can be precisely measured. “It’s like dropping a pebble in a bowl of Jell-O to measure the ripples created,” says Goodman. “This technique takes something that once was very qualitative (feeling stiffness) and enables us to put a number on it.”
The Wisconsin-UCSD Liver Study will be following 100 volunteers who are obese and already planning to undergo bariatric surgery. Patients will have these 3D elastography imaging scans conducted at multiple time points, as well as a tissue biopsy during surgery, to compare the two techniques. Since patients undergoing bariatric surgery often have positive metabolic changes that impact the health of their liver, the study will be a good opportunity to see if the imaging technique can detect changes induced by the surgical intervention. “It’s a nice model system to test drive the sensitivity of these advanced imaging techniques,” says Goodman.
Ultimately, these advanced techniques could potentially be used in clinical studies to see if medicines have a positive impact on patients. “It’s a way for us to enable science that is very directly related to patient care and gives us the ability to assess the efficacy of compounds in future studies,” says Goodman.





