A Novel Approach to Hemophilia: Stopping the Body’s Natural Clotting Brakes
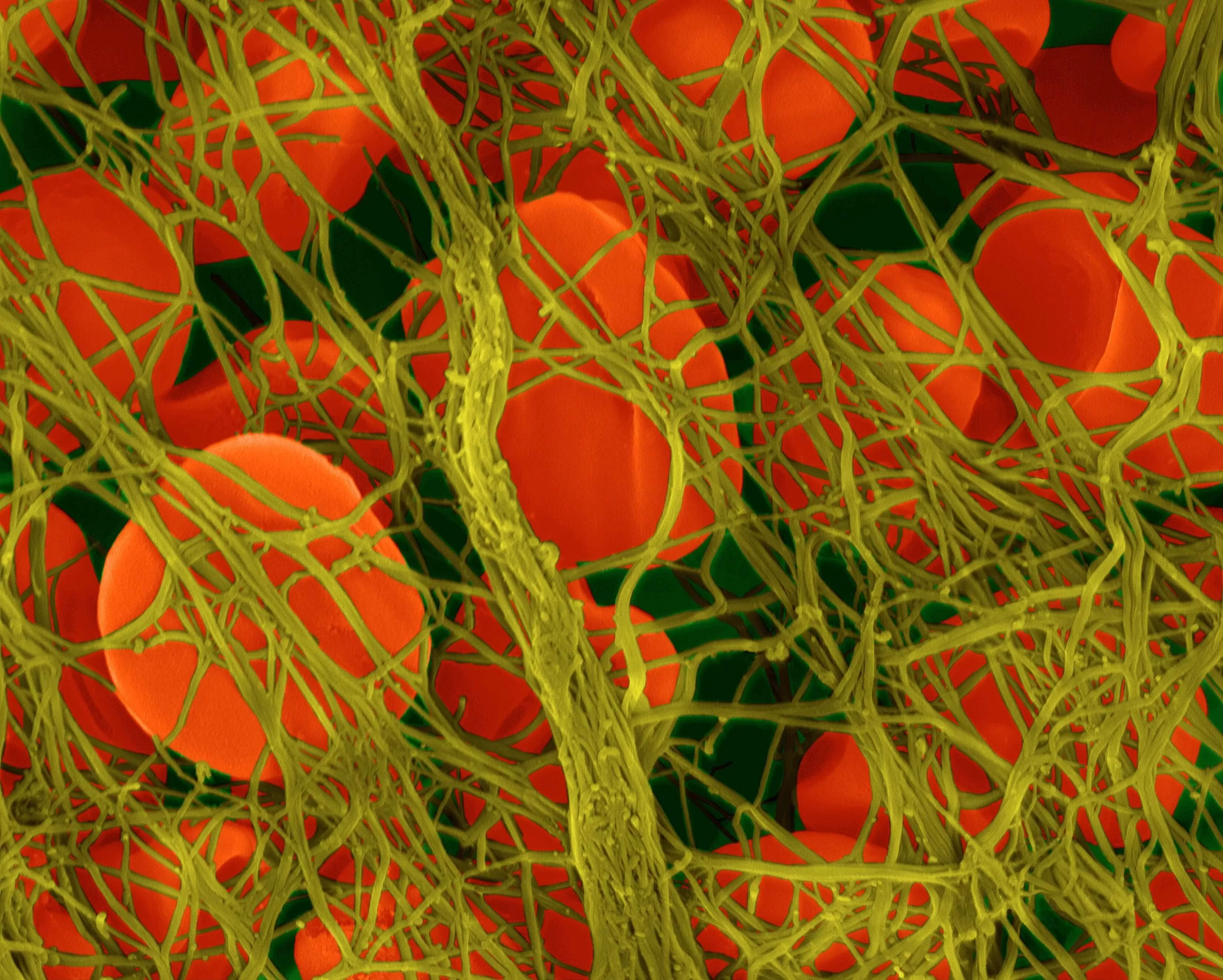
Our bodies delicately balance clotting and anti-clotting mechanisms, which help to stop bleeding when there’s an injury or dissolve dangerous clots that can form in blood vessels.
But for patients with hemophilia, a rare genetic disease that causes deficiencies in clotting factor VIII or IX, this delicate balance is upset. Patients experience excessive bleeding after an injury and can suffer permanent joint damage following repeated bleeding episodes. For decades, the most common treatment approach has been to replace the missing clotting factor in these patients, restoring the equilibrium.
These treatments with clotting factor, however, have drawbacks. Mainly, patients have to receive intravenous infusions usually one or three times a week to prevent bleeding. This adds up to between 50 and 150 infusions a year, says Steven Arkin, Executive Director of Pfizer’s Rare Disease Research Unit. Additionally, administering these treatments to children is particularly challenging because their veins are smaller and it’s difficult for them to sit still. “Children are the most active, and we want to protect their joints for a lifetime,” he adds.
A new pathway to restoring balance
In hopes of finding alternative pathways to treating hemophilia, Pfizer scientists are pursuing a completely new approach. Instead of adding back in missing or insufficient clotting factors, scientists are now focusing on the opposite side of the equation: inhibiting the body’s natural mechanisms that dissolve blood clots. One such target is tissue factor protein inhibitor (TFPI), a natural anti-coagulation protein that prevents blood clots. Scientists are developing a monoclonal antibody against TFPI, a type of protein drug that can bind to and inhibit the activity of TFPI. The administration of this medince would be more convenient for patients since it could be self-administed by injection.
In addition to the anti-TFPI program, Pfizer currently has two gene therapy programs in clinical testing that could treat hemophilia A and B respectively. In each these programs, an adeno-associated virus (AAV) has been engineered to deliver a healthy copy of a clotting factor gene. “We’re taking a multi-pronged approach to treating hemophilia,” says Arkin. “We hope to have therapies that meet the needs of every single hemophilia patient.”
Taking off the brakes
The body’s clotting mechanisms operate through two separate pathways that interact—the intrinsic and extrinsic pathways. When a person has a cut or injury, the extrinsic pathway is first triggered to kick start the clotting process, like turning on the pilot light on a stove. Then the intrinsic pathway, like turning up the gas, acts as an amplifier to fully stop the bleeding. Patients with hemophilia are missing parts of the amplification pathway. With an anti-TFPI therapeutic, scientist hope they can augment the extrinsic pathway, by removing the body’s natural anti-clotting mechanisms. “We’re taking off the breaks on the initiation signal so it can do the whole job of clotting itself without being amplified,” says Arkin.
In developing the protein therapy to target TFPI, scientists had somewhat of a “Goldilocks” scenario, says Arkin. They wanted it to bind with TFPI, but not too much to the point that it’s completely shut down. “Some of the art in developing this potential therapeutic was to design it to have just the right amount of affinity for the target,” he says. Ultimately, scientists have landed on what appears to be a “well-behaved” protein medicine, says Arkin.
And as a once-a-week subcutaneous injection, it’s a potentially more convenient option for patients, especially the youngest ones. “It’s a whole lot easier to get a needle under the skin for a child, then trying to get something into their vein,” says Arkin.