‘Bucket Brigades’ Gone Rogue: A New Path to Shutting Down Cancer Growth

A critical pathway in our cells acts like a bucket brigade, efficiently passing on signals that control cellular growth. But what happens when one set of “hands” on the line goes rogue?
The mitogen-activated protein kinase (MAPK) pathway is a chain of proteins that relays signals from outside the cell into the nucleus, controlling cellular growth and death. When this essential pathway malfunctions, it may lead to more than just chaos—it may determine how cancer progresses.
If one of these proteins along the chain is mutated, cells may proliferate uncontrollably, which may lead to cancer. One of the most well-known examples is the BRAF gene mutation, which affects some of those MAPK-pathway proteins. The BRAF gene is linked to multiple cancer types including melanoma, breast, ovarian, and colon cancers.
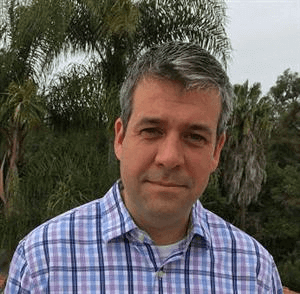
Nate Ihle.
While the MAPK “bucket brigade” has been a long-researched cancer target, in recent years scientists have focused on developing targeted therapies that seek to more precisely home in on the rogue members of the MAPK pathway to curb out-of-control cell growth. “[The MAPK pathway] is prominent in the growth and survival of tumor cells, but unfortunately, it’s also critical in normal cells, making it a challenge to inhibit,” says Nate Ihle, a Principal Scientist at Pfizer’s La Jolla, California site, whose research explores how to selectively turn off this pathway. Known as MAP-kinase inhibitors, these therapies are also being tested for use in combination therapies.
Finding the Right Way In
Part of fine-tuning MAP-kinase inhibitors is finding the best strategy for stopping the “bucket brigade.” It may start at the genetic level, finding the specific gene that is causing the pathway to go rogue. Or it may be targeting the specific “bucket holder,” the player along the pathway, such as a certain enzyme that’s overexpressed that leads to cellular overgrowth. “These pathways have so many elements. It could be the cancerous gene itself, it could be the player that the gene is selectively utilizing, or it could be a way of making the tumor more susceptible to the pathway inhibited,” says Ihle.
A Fine-Tuned Combination, for Better Quality of Life
What if therapies don’t kill all the cells? Such is the case with the “persisters,” a subset of cancer cells that play a sort of cat-and-mouse game when anti-cancer therapies are deployed. They may grow slowly after being exposed to a medicine and then acquire a mutation and swiftly proliferate again. When developing therapies to block MAPK pathways, combining it with other treatments may be the key to outsmarting these survivor cells. “You can hit the tumor with a signal transduction inhibitor, basically weaken the tumor, and then allow the immune system to come in and mop up the rest,” Ihle says.
Or using epigenetic strategies, the persisters can be put in a more sensitized state so they respond better to the therapy. “It’s triangulating,” Ihle says. “It’s taking the strength of each tool and optimizing it where you have this really dramatic effect.”
For Ihle, it’s not just about killing tumors, it’s about developing therapies that improve quality of life for cancer patients. “That’s what you are trying to do if you can attack a tumor in a specific way. You are trying to improve people’s lives,” he says.