What Is Lupus?
Lupus is a chronic autoimmune disease that causes inflammation as the immune system attacks healthy tissue all over the body. It primarily affects the skin, joints, and internal organs such as the kidney and heart. However, since it can impact many different areas of the body, symptoms vary widely.1
Lupus Prevalence
The Lupus Foundation estimates that about 1.5 million Americans and at least 5 million people around the world have some form of lupus. The disease primarily impacts those assigned female at birth (90%) during childbearing age, but those assigned male at birth, as well as children and teens, can develop the condition, too.2
A 2021 epidemiologic breakdown by racial and ethnic subpopulations in the United States demonstrates the prevalence of systemic lupus erythematosus (SLE), the most common form of lupus. In the study:3
- SLE was nine times higher in those assigned female at birth than those assigned male at birth.
- In those assigned female at birth, SLE was highest among American Indian/Alaska Natives and Black populations.
- American Indian/Alaska Native populations presented with the highest race-specific SLE estimates for lupus in all genders.
Causes and Risk Factors

What Causes Lupus?
Researchers haven’t identified the cause of lupus. But it's believed that this complex disease is linked to the interactions of hormones, genes, and environmental factors.4
Lupus and Genetics
More research is required to determine whether lupus is hereditary. A genetic link first gained attention because of lupus's tendency to cluster in families and show up more frequently in certain ethnic groups.1,4
Genes associated with the disease include:
- Genes that help to design or shape the immune system’s response to antigens by coding proteins, known as major histocompatibility complex (MHC) class II and III4
- Genes that code for receptors, which are immune proteins that attach or bind to a molecule that has an effect on cells. Examples of receptors that are affected in lupus in include complement (immune system proteins) receptors, antibodies, and Fc ɣ4
- Genes that code for variants of opsonins, compounds that allow the immune system to label and eliminate particles in a process called phagocytosis4
- Genes induced by immune system proteins such as type 1 interferons5,6
Lupus Risk Factors
Hormones and environmental factors may increase a person’s risk of getting lupus. For example, the higher incidence of lupus among those assigned female at birth is believed to be tied to higher quantities of estrogen, thanks to the hormone's "immune-enhancing" characteristics.4 Additionally, genes involved in innate immunity are linked to the X chromosome.6,7
Environmental factors have been elusive, but researchers have discovered connections between lupus and a range of toxins and infectious diseases, including:
- Silica4
- Mercury4
- Cigarette smoke4
- Viral and other infections, such as mononucleosis (caused by the Epstein-Barr Virus), shingles (caused by the herpes zoster virus), cytomegalovirus, hepatitis C, and papillomavirus4,8
Other factors with the potential to aggravate symptoms include certain drugs, ultraviolet light exposure, and stress.4
Types of Lupus
Lupus is the parent category for several more specific types of this disease.1
- Systemic Lupus Erythematosus (SLE)
Most frequently, people are referring to SLE when they say “lupus.” This type of lupus gets its name from its potential to affect multiple organ systems in the human body, including the joints, skin, and kidneys. It can also extend to the cardiovascular and nervous systems.9
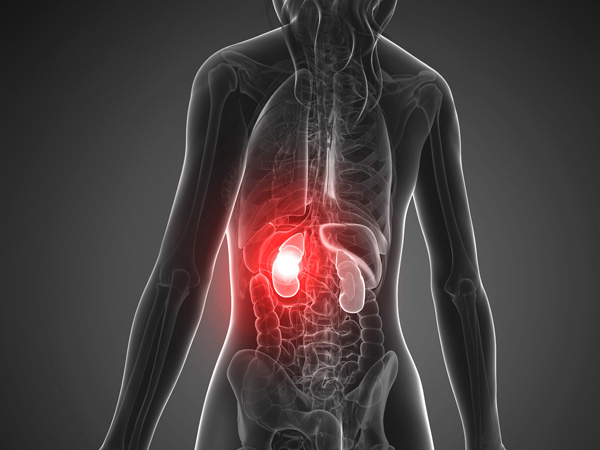
One of the most serious complications of SLE is lupus nephritis, which describes an immune system attack on the kidneys, leading to inflammation and the possibility of organ damage.10 Left untreated, symptoms can worsen and lead to kidney failure. If the condition becomes very serious, a patient may need dialysis or a kidney transplant.11
- Cutaneous Lupus Erythematosus (CLE)
CLE affects only the skin. Although the disease can occur in people without SLE, at least 5% of people who develop CLE may develop SLE at a later time.1,9
CLE consists of several sub-types. Acute cutaneous lupus erythematosus (ACLE), subacute cutaneous lupus erythematosus (SCLE), and chronic cutaneous lupus erythematosus (CCLE), which is also called discoid lupus erythematosus (DLE), are the most common.12,13
- Acute cutaneous lupus erythematosus (ACLE)
ACLE can be localized (occurring on one part of the body) or generalized (occurring on multiple parts). In localized form, ACLE typically takes the form of the butterfly rash (or malar rash). The rash’s duration can range from days to weeks, and sun exposure may cause it.13
- Subacute cutaneous lupus erythematosus (SCLE)
Like ACLE, SCLE is often triggered by sun exposure. But unlike ACLE, the rash typically occurs on upper parts of the torso and on the neck, back, and arms—not the face.13
- Chronic cutaneous lupus erythematosus (CCLE)
CCLE is also called discoid lupus erythematosus (DLE), and it is one of the most frequently encountered types of cutaneous lupus. DLE is a chronic skin condition that presents as sores with inflammation and scarring. It typically shows up around the face, ears, and scalp, although it can appear in other areas. The lesions are red, inflamed patches that appear thickened . The condition can cause permanent scarring and hair loss.13
- Childhood Lupus
Childhood lupus mirrors the effects of the adult form of the condition. But unlike adult lupus, childhood lupus is more common in those assigned male at birth. Childhood lupus also affects certain organs more significantly, including the kidneys. Children diagnosed with lupus develop kidney disease twice as often as adults with lupus.9
- Neonatal Lupus Erythematosus (NLE)
NLE occurs when a mother transfers autoantibodies of Sjogren syndrome to an unborn baby. Those autoantibodies include autoantigen type A (Ro/SSA) or autoantigen type B (La/SSB).14 These antibodies occur in about 1 in 1,000 healthy individuals, meaning that a pregnant person who has a child with neonatal lupus may not have the disease themselves.9 Although rare, NLE can include rashes and cardiac issues.9,14
- Drug-Induced Lupus Erythematosus
While the general cause of lupus is unknown, some drugs can trigger lupus-like symptoms, even in people who don't have SLE. Unlike other types of lupus, drug-induced lupus erythematosus is transient. Discontinuing the drug causing the condition usually resolves the rash in a matter of months. Additionally, doctors are increasingly avoiding medications known to induce lupus.9
These medications include:9
- Certain blood pressure medications, such as hydralazine and methyldopa
- Procainamide, a heart medication
- D-penicillamine, which is used to treat metal poisoning
- Minocycline, a common acne treatment
Lupus Symptoms
Part of the challenge of diagnosing lupus is that its symptoms vary. They may fluctuate over time during and between flare-ups. Symptoms range from mild to severe and may affect just one area of the body or multiple systems at a time. Symptoms often show up alongside the disease-causing inflammation of particular organs such as the skin, lining of heart and lungs, kidneys, joints, brain, and even blood cells.18
SLE diagnostic criteria can include:19
- Malar rash, which commonly appears on the face and is also known as a butterfly rash.13,19
- Discoid rash, which includes sores that appear on the mouth, face, and other parts of the body. They may be red, scaly, or thick, leaving skin discolored or scarred when they clear.12,13,19
- Sores in the nose and mouth13,19
- Arthritis of the arms or legs19
- Pleuritis (inflammation of tissue that lines the lungs and chest) or pericarditis (inflammation of the sack that encases the heart)19
- Kidney disorder19
- Neurological disorders, including seizures or psychoses19
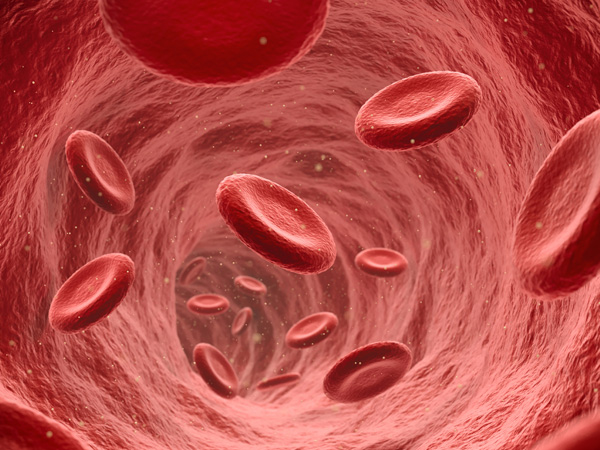
- Hematological disorders, including hemolytic anemia with reticulocytosis (a condition in which red blood cells are destroyed before their normal lifespan is up), leukopenia (a shortage of white blood cells), lymphopenia (a shortage of another type of white blood cells, lymphocytes), or thrombocytopenia (a shortage of blood platelets)19,20,21,22,23
Lupus Complications
Because lupus promotes inflammation in the body, it can also cause other health issues, including:
- Lupus nephritis, in turn leading to kidney damage18
- Heart problems, such as inflammation-related damage to heart valves, inflammation of the tissue around the heart (pericarditis), or inflammation of the muscular tissue of the heart (myocarditis)18
- Vasculitis, the inflammation of the blood vessels18
- Pleurisy from tissue inflammation surrounding the lungs18
- Bone weakness as a result of the use of glucocorticoids24
Lupus may increase a person’s chances of developing other conditions. For instance, inflammation of tissues in the heart and blood vessels may encourage cardiovascular disease, which can then cause atherosclerosis, or plaques in the blood vessels, as well as coronary artery disease, or plaques in the arteries directly near the heart.18
Less common symptoms include fainting spells, memory loss, and diminishing cognitive abilities. Because none of these signs indicate lupus on their own, they are evaluated within the context of other symptoms to determine whether someone might have lupus.25
Although lupus is more common among those assigned female at birth, those assigned male at birth who have lupus are more likely to have serious symptoms, including kidney, heart, lung, and blood issues, as well as antiphospholipid antibody syndrome and pain while taking deep breaths (pleurisy from serositis ). There is minimal research into how lupus affects transgender and nonbinary people, but it is believed that exogenous hormone therapy (such as estrogen therapy) could affect the condition.26
Lupus disproportionately affects people of color. For example, in people assigned female at birth, lupus occurs three times as often in African American people than in white counterparts.27 People of color are also at heightened risk for severe cases of SLE. Black people face higher mortality rates and earlier lupus deaths compared with white people.28
Diagnosis and Treatment
Lupus Diagnosis
Lupus is difficult to diagnose because its symptoms are often mistaken for those of other diseases. As a result, many people have lupus for a long time before receiving a formal diagnosis.15
There is no single test for lupus, so diagnostic criteria are broad. However, there are ways of determining a patient's status:
- Reviewing medical history
This involves talking to a doctor about symptoms and other associated problems. Noting symptoms, especially highlighting when and for how long they occur, is useful.15
- Assessing family history
Doctors will want to know if a patient has a family history of lupus or other autoimmune diseases.15
- Physical exams
In a physical exam, a doctor will look for rashes or other symptoms associated with lupus.15
- Lupus blood and urine tests
As an initial blood test , an antinuclear antibody (ANA) test can show whether a patient's immune system is more likely to create lupus autoantibodies. While most people with lupus have a positive test for ANA, a positive result doesn't mean someone definitely has lupus. After a positive test result, a doctor will order more tests for antibodies that are specific to SLE and may conduct urine tests to screen and monitor for kidney dysfunction.15,16
- Anticoagulant tests
Coagulation tests are used to identify the lupus anticoagulant. If lupus anticoagulant is present, the blood will take longer than normal to clot during the coagulation test. The lupus anticoagulant is a type of antiphospholipid (APL) antibody, which roughly half of all lupus patients have, making APL useful in the initial diagnosis of lupus. Other APL tests include anticardiolipin antibody and anti-beta2 glycoprotein 1.15,17
- Skin and kidney biopsies
This method involves minor surgery to obtain tissue samples. These samples are then examined under a microscope to look for signs of autoimmune disease.15
Lupus is difficult to diagnose, and symptoms can change over time. People living with lupus and their loved ones may, therefore, experience uncertainty and frustration. However, in some cases, treatments are available to help manage the disease and promote a higher quality of life . Most lupus treatments are the same regardless of gender or sex.26
Finding a healthcare provider who listens to patient concerns is critical in treating lupus. Most patients will see a rheumatologist, but many people see other specialists as well if they experience damage to specific organs.29
Lupus patients and their caregivers will work with physicians and other clinicians to develop the best treatment plan and outcome goals. The goals of this plan, in addition to general healthcare, will often include:29
- Reducing inflammation
- Controlling symptoms like joint pain
- Preventing flare-ups and finding ways to treat them when they do occur
- Minimizing organ damage
- Suppressing an overactive immune system
Determining the right combination of medicines that best control patient symptoms can take months or longer.29 Currently, there are a handful FDA-approved medications for treating lupus:
- An antimalarial drug30
- An immunosuppressant31
- A calcineurin inhibitor32
- A biologic, monoclonal antibody approved for adults who have moderate to severe SLE and are receiving other standard treatments.33
Doctors will often prescribe other medications off-label as part of the normal standard of care.34,35 Some of these treatments include:29,34,35
- Corticosteroids
- Antimalarials
- Immunosuppressives
- Anticoagulants
Additional medical treatments also include therapies such as diuretics, anticonvulsants, antibiotics, and bone-strengthening drugs to combat osteoporosis.29
Since lupus is a systemic disease, strong nutritional habits as part of a treatment plan may optimize a patient's overall health.36
It’s recommended that people who have lupus eat a healthy, balanced diet, limiting the consumption of highly processed foods. The Lupus Foundation of America provides tips for eating healthy for those who have lupus.37
Patients with lupus may experience weight gain or loss as their appetite, dietary habits, possible use of steroids, energy levels, and mobility all change. Those with lupus who are between the ages of 35 and 44 and were assigned female at birth have a heart attack risk that's 50 times greater than the risk in the general population, underlining the benefits for them in particular of a diet lower in saturated fats, cholesterol, and sodium.36
Some drugs used to treat lupus, including corticosteroids, acetaminophen, and warfarin, can interact with alcohol, meaning that people with lupus may need to limit their alcohol intake to protect the liver and stomach. Taking some drugs, such as certain immunosuppressants, means that patients cannot consume alcohol at all.36 Patients should consult with a healthcare professional to better understand potential drug interactions.
Global Impact of Lupus
Lupus is a global disease that affects an estimated 5 million people worldwide, with 16,000 new cases being discovered per year in the United States alone.2 Its prevalence varies significantly between regions. Over the past several decades, researchers have found the highest prevalence and incidence of SLE specifically in North America, with the lowest incidences reported in Africa and Ukraine. The lowest prevalence has been found in Northern Australia.38 Although data is limited, SLE specifically is reported to be more common and severe among people of African and Asian descent who reside in industrialized countries.39

Lupus Inequities
One study assessed communication among patients with lupus and providers, using the following information:
- How patients self-managed their medications and treatments
- How the patients perceived their overall health
- Information from visits with healthcare providers
After comparing information from different racial groups, researchers found that African Americans who had serious cases of lupus reported rushed communication with their healthcare providers. Moreover, African Americans who said their healthcare providers communicated poorly also had more lupus-related damage—a finding they did not share with white patients. The same study found that younger white people experienced less lupus-related damage than their Black counterparts.40
Frequently Asked Questions About Lupus
- Is lupus contagious?
Lupus cannot be caught or spread. It is not transmissible through sexual contact, either. The virus is the product of several factors, including the environment, hormones, and genetics.41
- Can you die from Lupus?
If left untreated,or in patients with frequent and very severe symptoms, lupus can cause life-threatening problems. However, if patients receive consistent treatment and follow-ups, as many as 90% can expect to live a normal life.42
- Is lupus a type of cancer? Are lupus patients more likely to get cancer?
Lupus is not a type of cancer, but research indicates that people with lupus have a slightly heightened risk of developing cancer compared with people who do not have lupus. For example, for people with lupus, the risk of developing non-Hodgkin's lymphoma is four times that of people who do not have lupus. At the same time, it's associated with a decreased risk of other cancers, including breast cancer.43
- Does lupus go away on its own?
No. Lupus is a chronic disease, and it does not go away on its own. However, effective treatments can lessen symptoms and minimize complications. A notable exception is drug-induced lupus, which usually disappears after the drug is stopped (if this is possible). Research to determine a cure for lupus is underway.44
- Is there a Lupus diet?
Following general nutrition tips has overall health effects that can benefit anyone with lupus. Talk with a doctor or nutritionist to find a plan that best fits the symptoms of your disease and your specific nutritional needs.36,37
Learn More About Lupus
Explore lupus clinical trials at ClinicalTrials.gov.
Area of Focus: Inflammation & Immunology
Lupus is a focus of Pfizer’s Inflammation & Immunology Therapeutic Area. Visit the Inflammation & Immunology Page.
- References
- What is lupus? Lupus Foundation of America. Accessed February 7, 2022. https://www.lupus.org/resources/what-is-lupus.
- Lupus facts and statistics. Lupus Foundation of America. Accessed February 7, 2022. https://www.lupus.org/resources/lupus-facts-and-statistics.
- Izmirly PM, Parton H, Wang L, et al. Prevalence of systemic lupus erythematosus in the united states: estimates from a meta‐analysis of the centers for disease control and prevention national lupus registries. Arthritis & Rheumatology. 2021;73(6):991-996. doi:10.1002/art.41632. Published April 23, 2021.
- Causes of lupus. Johns Hopkins Lupus Center. Accessed February 14, 2022. https://www.hopkinslupus.org/lupus-info/lupus/.
- Postal M, Vivaldo JF, Fernandez-Ruiz R, Paredes JL, Appenzeller S, Niewold TB. Type I interferon in the pathogenesis of systemic lupus erythematosus. Current Opinion in Immunology. 2020;67:87-94.
- Odhams CA, Roberts AL, Vester SK, et al. Interferon inducible X-linked gene CXorf21 may contribute to sexual dimorphism in Systemic Lupus Erythematosus. Nat Commun. 2019;10(1):2164.
- Jaillon S, Berthenet K, Garlanda C. Sexual dimorphism in innate immunity. Clinic Rev Allerg Immunol. 2019;56(3):308-321.9.
- Quaglia M, Merlotti G, De Andrea M, Borgogna C, Cantaluppi V. Viral infections and systemic lupus erythematosus: new players in an old story. Viruses. 2021;13(2):277.
- Types of lupus. Johns Hopkins Lupus Center. Accessed February 7, 2022. https://www.hopkinslupus.org/lupus-info/types-lupus/.
- Lupus nephritis. Symptoms & causes. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/lupus-nephritis/symptoms-causes/syc-20354335. Accessed July 21, 2022.
- Lupus nephritis. Diagnosis & treatment. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/lupus-nephritis/diagnosis-treatment/drc-20446438. Accessed July 21, 2022.
- Eastham AB, Vleugels RA. Cutaneous lupus erythematosus. JAMA Dermatol. 2014;150(3):344.
- Cooper EE, Pisano CE, Shapiro SC. Cutaneous manifestations of “lupus”: systemic lupus erythematosus and beyond. Rothschild BM, ed. International Journal of Rheumatology. 2021;2021:1-19.
- Diaz-Frias J, Badri T. Neonatal lupus erythematosus. StatPearls. National Library of Medicine. Updated June 27, 2022. Accessed September 26, 2022. https://www.ncbi.nlm.nih.gov/books/NBK526061/.
- Diagnosing and treating lupus. Centers for Disease Control and Prevention. Updated October 17, 2018. Accessed February 7, 2022. https://www.cdc.gov/lupus/basics/diagnosing.htm.
- Lab tests for lupus. Lupus Foundation of America. Updated July 15, 2013. Accessed November 29, 2022. https://www.lupus.org/resources/lab-tests-for-lupus.
- Antiphospholipid antibodies. Johns Hopkins Lupus Center. Accessed December 7, 2022. https://www.hopkinslupus.org/lupus-tests/antiphospholipid-antibodies/.
- Systemic lupus erythematosus (lupus). National Institute of Arthritis and Musculoskeletal and Skin Diseases. Updated June 2019. Accessed February 7, 2022. https://www.niams.nih.gov/health-topics/lupus.
- Aringer M, Costenbader K, Daikh D, et al. 2019 European League Against Rheumatism/American College of Rheumatology Classification Criteria for Systemic Lupus Erythematosus. Arthritis & Rheumatology. 2019;71(9):1400-1412. . https://www.rheumatology.org/portals/0/files/1997%20update%20of%201982%20revised.pdf.
- Baldwin C, Pandey J, Olarewaju O. Hemolytic Anemia. StatPearls. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK558904/. Updated July 25, 2022. Accessed November 29, 2022.
- Leukopenia. National Cancer Institute. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/leukopenia. Accessed November 29, 2022.
- What is lymphopenia? National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health/lymphopenia. Updated May 31, 2022. Accessed November 29, 2022.
- Platelet disorders. Thrombocytopenia. National heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health/thrombocytopenia. Updated March 24, 2022. Accessed November 29, 2022.
- Stojan G, Petri M. The risk benefit ratio of glucocorticoids in SLE: Have things changed over the past 40 years? Curr Treat Options in Rheum. 2017;3(3):164-172.
- What to do about uncommon symptoms. Lupus Foundation of America. Accessed February 7, 2022. https://www.lupus.org/resources/what-to-do-about-uncommon-symptoms.
- What role do sex and gender play in lupus? Lupus Foundation of America. Accessed November 30, 2022. https://www.lupus.org/resources/what-role-do-sex-and-gender-play-in-lupus.
- African Americans and Lupus. Lupus.org. Accessed July 22, 2022. https://www.lupus.org/s3fs-public/Doc%20-%20PDF/Ohio/African%20Americans%20and%20Lupus.pdf.
- Drenkard C, Lim SS. Update on lupus epidemiology: Advancing health disparities research through the study of minority populations. Current Opinion in Rheumatology. 2019;31(6):689-696.
- Finding the treatment approach for you. Lupus Foundation of America. Accessed February 7, 2022. https://www.lupus.org/resources/finding-the-treatment-approach-for-you.
- Lupus therapies continue to evolve. U.S. Food & Drug Administration. https://www.fda.gov/consumers/consumer-updates/lupus-therapies-continue-evolve. Updated August 31, 2021. Accessed November 3, 2022.
- FDA approves first treatment for pediatric patients with lupus. U.S. Food & Drug Administration. https://www.fda.gov/news-events/press-announcements/fda-approves-first-treatment-pediatric-patients-lupus. Updated April 26, 2019. Accessed November 3, 2022.
- Heo YA. Voclosporin: First approval. Drugs. 2021;81(5):605-610.
- Deeks ED. Anifrolumab: First approval. Drugs. 2021;81(15):1795-1802.
- Fanouriakis A, Kostopoulou M, Alunno A, et al. 2019 update of the EULAR recommendations for the management of systemic lupus erythematosus. Annals of the Rheumatic Diseases. 2019;78(6):736-745.
- Fanouriakis A, Tziolos N, Bertsias G, Boumpas DT. Update οn the diagnosis and management of systemic lupus erythematosus. Annals of the Rheumatic Diseases. 2021;80(1):14-25.
- Diet. Johns Hopkins Lupus Center. Accessed February 7, 2022. https://www.hopkinslupus.org/lupus-info/lifestyle-additional-information/lupus-diet/.
- Eating healthy when you have lupus. Lupus Foundation of America. Updated May 23, 2022. Accessed September 27, 2022. https://www.lupus.org/resources/diet-and-nutrition-with-lupus.
- Rees F, Doherty M, Grainge MJ, Lanyon P, Zhang W. The worldwide incidence and prevalence of systemic lupus erythematosus: A systematic review of epidemiological studies. Rheumatology. 2017;56(11):1945-1961. doi:10.1093/rheumatology/kex260.
- Tikly M, V Navarra S. Lupus in the developing world – is it any different? Best Practice & Research Clinical Rheumatology. 2008;22(4):643-655. doi:10.1016/j.berh.2008.05.003.
- Sun K, Eudy AM, Criscione-Schreiber LG, et al. Racial differences in patient-provider communication, patient self-efficacy, and their associations with systemic lupus erythematosus–related damage: a cross-sectional survey. J Rheumatol. 2021;48(7):1022-1028.
- Is lupus contagious? Lupus Foundation of America. Accessed February 7, 2022. https://www.lupus.org/resources/is-lupus-contagious.
- Prognosis and life expectancy. Lupus Foundation of America. Accessed February 7, 2022. https://www.lupus.org/resources/prognosis-and-life-expectancy.
- Ladouceur A, Tessier-Cloutier B, Clarke AE, et al. Cancer and systemic lupus erythematosus. Rheumatic Disease Clinics of North America. 2020;46(3):533-550. doi:10.1016/j.rdc.2020.05.005.
- Frequently asked questions | lupus center. Cincinnati Children's Hospital Medical Center. Accessed February 7, 2022. https://www.cincinnatichildrens.org/service/l/lupus/faq
The information contained on this page is provided for your general information only. It is not intended as a substitute for seeking medical advice from a healthcare provider. Pfizer is not in the business of providing medical advice and does not engage in the practice of medicine. Pfizer under no circumstances recommends particular treatments for specific individuals and in all cases recommends consulting a physician or healthcare center before pursuing any course of treatment.
Related Articles
Lupus and Pregnancy: What You Need to Know
There was a time when women were told that pregnancy was impossible if they had lupus. While all lupus pregnancies are still considered high risk, advances in medical technology and in our understanding of the disease have made it possible for women with lupus to have successful pregnancies. But...
Consumer DNA Kits Give Research a Boost
At-home DNA tests are driving patient participation in research. DNA kits can trace more than your ancestry. They’re also helping medical research. Patients with lupus and inflammatory bowel disease (IBD) recently became a pivotal part of studies without ever stepping foot in a clinic or hospital...



