Disease Education Information
Treating a Rare Lung Disease
Lymphangioleiomyomatosis (LAM) is a rare, progressive, cystic disease of the lungs. It is associated with declining lung function and almost exclusively affects women. The average age of diagnosis is approximately 35 years.1,2
- What is LAM?
LAM is a genetic disease that can be inherited with tuberous sclerosis complex (TSC-LAM) or can be sporadic (S-LAM). It is caused by mutations in genes called tuberous sclerosis complex genes (TSC1 or TSC2).1 This results in a deficiency or dysfunction of the genes’ protein products, hamartin or tuberin, which leads to inappropriate cell growth and proliferation, particularly of smooth muscle-like cells called LAM cells, which infiltrate the lungs and lymphatics.3 Changes in the lungs obstruct air flow and can lead to other significant, potentially life-threatening problems.1
- Who gets LAM?
TSC-LAM occurs in up to 40% of women with tuberous sclerosis complex,4 while S-LAM affects approximately three to five women per million in the general population.5
- What are the Symptoms of LAM?
Patients affected by LAM most commonly develop progressive shortness of breath with exertion, recurrent cases of collapsed lung (pneumothorax), and chylous fluid collections around the lungs.1
On average, women with LAM may have symptoms for three to five years,6 and may have had two or more incidents of pneumothorax before the diagnosis is made.7 In patients with this disease, lung function tests show reduced air flow rates and diffusion capacity. Patients can also have rare abdominal tumors that include angiomyolipomas of the kidney and lymphangiomyomas.1
- How is LAM Diagnosed?
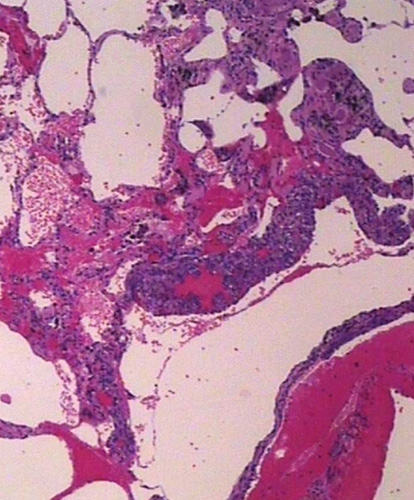
Pulmonary LAM can be diagnosed using high-resolution CT imaging, which will typically show round, thin-walled cysts throughout the lungs, together with some features of TSC.1,2
A lung biopsy may be required for diagnosis in cases in which TSC is absent. A blood test for a biomarker called serum vascular endothelial growth factor-D may also be helpful in the diagnosis of LAM because levels of that factor have been found to be elevated in most women who have LAM.1,2
- Can LAM be Treated?
In some countries, there is an approved therapy for patients with LAM that has been shown to stabilize lung function. This therapy belongs to a class of medications called mTOR inhibitors, which block cell growth and proliferation.2,7
Other types of medications have been used in the treatment of LAM, although they remain unproven. Supportive care may include supplemental oxygen. If lung function markedly declines, lung transplantation may be an option for some patients.2,7
Lymphangioleiomyomatosis (LAM) Resources
Area of Focus: Rare Disease
Lymphangioleiomyomatosis (LAM) is a focus of our Rare Disease Therapeutic Area.
Visit Our Rare Disease Site DetailsClinical Trials
We proudly partner with thousands of study sites and tens of thousands of trial participants around the world. It's these clinical trials that lead to life-changing medicines.
Go to Pfizer Clinical Trials Site DetailsReferences
1. National Organization of Rare Disorders. Lymphangioleiomyomatosis. https://rarediseases.org/rare-diseases/lymphangioleiomyomatosis/. Accessed February 10, 2020.
2. NIH National Heart, Lung, and Blood Institute. LAM. https://www.nhlbi.nih.gov/health-topics/lam. Accessed February 10, 2020.
3. Krymskaya V. Smooth Muscle-Like Cells in Pulmonary Lymphangioleiomyomatosis. Proc Am Thorac Soc. 2008;5(1):119-126.
4. Cudzilo C, McCormack F, et al. Lymphangioleiomyomatosis Screening in Women With Tuberous Sclerosis. Chest. 2013;144(2):578-585.
5. Lymphangioleiomyomatosis (LAM). Breathe (Sheff). 2017;13(1):64–71.
6. Rare Diseases Clinical Research Network. What is Lymphangioleiomyomatosis (LAM)? https://www.rarediseasesnetwork.org/cms/rld/Learn-More/Disorder-Definitions. Accessed February 10, 2020.
7. The LAM Foundation. Diagnosing LAM. https://www.thelamfoundation.org/Healthcare-Providers/Diagnosis-Treatment/Diagnosing-LAM. Accessed February 10, 2020.