- Home
- Science
- Diseases & Conditions
- Leukemia
What Is Leukemia?
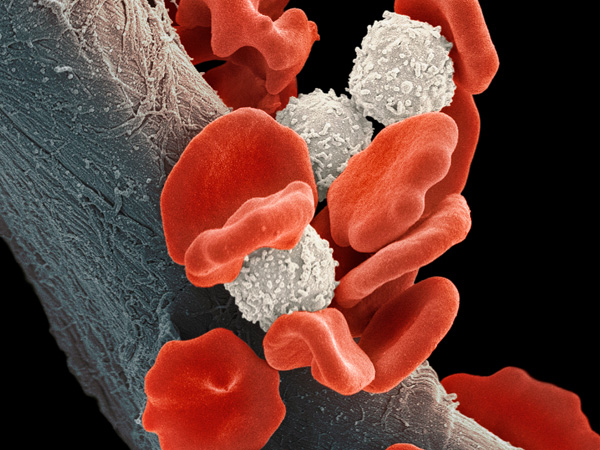
Leukemia is a broad term for blood cancers.1 The term applies to all types of leukemia, which include acute lymphocytic leukemia (ALL), acute myeloid leukemia (AML), chronic lymphocytic leukemia (CLL) and chronic myeloid leukemia (CML).1 Leukemia begins in the soft, spongy tissue that makes up the center of most bones, called bone marrow. Bone marrow produces several types of blood cells, which perform different functions:1
- White blood cells, which fight infection
- Red blood cells, which transfer oxygen from the lungs to the rest of the body
- Platelets, which form clots that stop bleeding
In leukemia patients, the bone marrow produces large amounts of abnormal blood cells, which make it hard for healthy cells to do their important jobs. Over time, the cancerous cells can also spread to other organs and tissues throughout the body.1
Leukemia Prevalence
Approximately 472,714 Americans have leukemia.2 The American Cancer Society (ACS) predicts 60,650 new leukemia diagnoses in 2022 and roughly 24,000 deaths from the disease.3 Among adults in the U.S., leukemia is the eleventh most common cancer, accounting for 3.2% of all new cancer diagnoses and 3.9% of all cancer deaths.2 Leukemia generally affects more adults than children, with most diagnoses occurring between the ages of 65 and 74.2
Leukemia Prognosis
The prognosis for leukemia has improved dramatically in recent decades thanks to groundbreaking genetic research and new treatment options. On average, the overall five-year survival rate for adults with leukemia is more than 66%.4 The survival rates for specific types of leukemia are as follows:4
- Acute lymphocytic leukemia (ALL): 72.1%
- Acute myeloid leukemia (AML): 29.8%
- Chronic lymphocytic leukemia (CLL): 88.6%
- Chronic myeloid leukemia (CML): 71.7%
Frequently Asked Questions About Leukemia
- Is leukemia curable?
Remission of leukemia is possible with treatment.56,57,58,59,60 The survival rate depends on how the disease progresses. On average, the five-year survival rate for people with leukemia is 66%, while 94% of children under 5 and 93% of adolescents under 15 recover after treatment.4
- Is it possible to beat or survive leukemia?
Yes. After diagnosis and treatment, some people with leukemia will experience remission, which means leukemia can no longer be detected in their body. However, it is possible for leukemia to recur.56,57,58, 59,60
- Is leukemia genetic?
Leukemia is caused by genetic changes in blood cells produced in bone marrow cells, but all known leukemia-causing genetic mutations are acquired during life, not inherited. However, certain inheritable genetic syndromes can increase the risk for acute leukemia. Having a close relative (especially an identical twin) with leukemia is a risk factor for developing leukemia.6,7,8,9,10,11,12
- What is the first sign of leukemia?
With fast-growing acute leukemias, the first symptoms are typically caused by a shortage of healthy blood cells. This can cause a patient to feel fatigued, dizzy, lightheaded, cold, or short of breath; experience bleeding or bruising easily; and have persistent or recurring infections. In slower-growing chronic leukemias, you might not experience any symptoms before diagnosis, but will have abnormal blood cell counts on lab tests.1-37
- What tests are necessary to diagnose leukemia?
Blood tests that measure the white blood cell, red blood cell, and platelet counts. Genetic testing can also help identify and classify the disease.1
- How high are monocytes in leukemia?
With CMML, the body produces too many monocytes—1,000 or more per cubic millimeter—which also elevates the total white blood cell count.26
- What types of doctors treat leukemia?
Hematologists (blood disorder specialists)61 and oncologists (cancer specialists)62 may be involved in treating a leukemia patient. Typically, if a doctor or other primary care provider suspects leukemia, they will refer patients to a hematologist or oncologist for a definitive diagnosis and treatment.63
Types of Leukemia
Leukemias are grouped into two categories: acute leukemia and chronic leukemia. The distinction is based on which blood cells are involved and how fast abnormal cells multiply.1 Acute leukemia develops and worsens quickly, while chronic leukemia develops slowly and worsens over time.1,13
Affected blood cells can either be lymphocytes (a type of white blood cell) or myeloid cells (immature cells that could develop into white or red blood cells or platelets). The type of leukemia a person has is determined in part by the affected cells: lymphocytes or myeloid cells.1
There are several different types of leukemia. Each has different treatment options and prognoses.
Also known as acute lymphoblastic leukemia, ALL progresses quickly and becomes fatal in just a few months if not treated.5 It begins in the bone marrow and affects white blood cells called lymphocytes—the main cells that comprise lymph nodes, a critical part of the immune system. There are two types of lymphocytes: B cells, which make antibodies to fight diseases, and T cells, which destroy germs and help regulate other immune system cells. B cell ALL begins in immature B cells, while T cell ALL can begin in T cells at any stage of maturity.14
ALL is uncommon, representing only about 0.5% of all cancers. ALL is most common in children younger than age 5, but ALL in adults is more fatal. Adults account for only 40% of ALL cases but 80% of deaths.15 Overall, the ACS predicts there will be 6,660 new cases of ALL in 2022 and 1,560 deaths.3
AML develops in immature myeloid cells.16 This type of leukemia typically affects older adults, who don't respond as well to treatment as children or adults under 60 do.17
The average age for receiving an AML diagnosis is 68, and the five-year AML survival rate is 26% for people older than age 20.18 Although AML is among the most common types of leukemia in adults, it only accounts for about 1% of all cancers. Overall, approximately 20,050 cases of AML will be diagnosed in 2022, and 11,540 people (almost all adults) will die from the disease.18
The most common leukemia in adults, CLL develops in lymphocytes and builds up slowly, often with no symptoms for the first few years.19 As the abnormal cells accumulate, they eventually spill into the bloodstream and spread to the lymph nodes, liver, spleen, and other parts of the body. This makes CLL and other chronic leukemias more difficult to diagnose and treat than acute leukemias.19
Typically, CLL starts in B cell lymphocytes, but there are a few rare types of CLL that behave differently:19
- Prolymphocytic leukemia (PLL) forms in immature B lymphocytes or T lymphocytes and typically grows and spreads faster than in common CLL. PLL tends to be more aggressive, and patients are more likely to relapse after treatment.
- Large granular lymphocyte (LGL) leukemia produces larger cancer cells than common CLL and has features of either T lymphocytes or another type of lymphocyte, natural killer cells. Most LGL leukemias grow slowly, but some are aggressive and difficult to treat.
- Hairy cell leukemia (HCL) develops into B lymphocytes that are different from common CLL B cells. Under a microscope, these cells look "hairy.” HCL is more treatable than other rare forms of CLL.
About 25% of leukemia diagnoses are some form of CLL, which almost always affects older adults. In 2022, experts projected roughly 20,160 new cases of CLL with 4,410 deaths.20Also known as chronic myelogenous leukemia, CML affects immature myeloid cells.21 In these cells, a genetic change produces an abnormal gene called BCR-ABL. This change turns the cells into CML cells.21 These cells multiply and accumulate, eventually spilling from bone marrow into the bloodstream and then to the spleen and other parts of the body. CML typically grows slowly.21 In more than 90% of cases, physicians catch the disease in its early stage, called the chronic phase.22 If untreated, CML can reach its accelerated phase and/or blast phase,23 which are more difficult to treat.21
CML occurs mostly in older adults and accounts for about 15% of new leukemia diagnoses. In 2022, roughly 8,860 people will be diagnosed with CML, and it will contribute to 1,120 deaths.24 The current 10-year survival rate for CML’s most common form is about 85%, and many patients have lifespans that are comparable to healthy adults.25
CMML is caused by an overproduction of abnormal white blood cells, especially monocytes. Healthy monocytes help protect the body against bacteria. With CMML, the monocyte count is abnormally high, which makes the overall white blood cell count too high. This may cause spleen enlargement. Between 15% and 30% of people with CMML eventually develop AML as well.26
CMML is extremely rare and accounts for only 1,100 new leukemia diagnoses in the U.S. each year.27 Of those, 90% are aged 60 or older.27
Most leukemias diagnosed in children are acute. Chronic leukemias are very rare in children.28 The disease has an occurrence rate of 4.9 cases in every 100,00 children and teens ages 0 to 19.29 Death rates for childhood leukemia have decreased by 84% since 1970.30
ALL is the most common leukemia in children, accounting for roughly 75% of childhood diagnoses. The rest are mostly AML. In rare cases, children can have mixed-lineage leukemia—cancer that has features of both AML and ALL. Or they may have juvenile myelomonocytic leukemia (JMML), cancer that begins in myeloid cells but grows slower than AML and faster than CML.28,31
Overall, leukemia accounts for nearly 1 in 3 cancer diagnoses among children and teenagers, making it the most common cancer for this age group, though it is still considered a rare disease. ALL is most common in children between ages 2 and 5 while AML is most common in children younger than age 2 and teenagers.31
Leukemia Symptoms

Different types of leukemia cause many of the same symptoms, but some types of leukemia have specific symptoms and potential complications. Leukemia symptoms in adults and children may vary.
Signs of Leukemia in Adults
Acute leukemias cause many of the same symptoms.32,33 Abnormal cells crowd out healthy blood cells and may cause a person to experience:32,33
- Feeling fatigued, dizzy, lightheaded, or cold
- Shortness of breath
- Pale skin
- Headaches
- Recurring infections or difficulty recovering from infections
- Bruises or tiny red or purple spots on the skin
- Bleeding, including frequent or severe nosebleeds, bleeding gums, or heavy menstrual bleeding
- Weight loss
- Fever
- Night sweats
- Loss of appetite
- Abdominal swelling or a feeling of fullness caused by an enlarged liver or spleen
- Enlarged lymph nodes
- Bone or joint pain
Chronic leukemias (CML, CLL, and CMML) can cause symptoms similar to those experienced with acute leukemias, but because these conditions develop much more slowly, people often experience no symptoms before a diagnosis. The most common sign of chronic leukemias is abnormal white or red blood cell counts.34,35,36 With CMML, extremely high monocyte levels show on blood tests. With CMML, monocytes can build up in the spleen or liver and enlarge these organs, causing a person to have abdominal pain or feel too full when eating.36
Signs of Leukemia in Children
The signs of leukemia in children are similar to those in adults.37 In rare cases, children might also experience seizures and vomiting.
In children, leukemia-like symptoms are more likely to be caused by other conditions. But it's important to have them seen by a doctor, who can perform blood tests to rule out leukemia or diagnose and treat it.
Leukemia Spots
Among the most visible signs of blood cancer are leukemia petechiae and leukemia purpura spots on the skin. Petechia are groups of pinpoint spots (smaller than 2 millimeters) that are nonblanching, meaning they do not disappear after applying brief pressure to the area. A purpura is a nonblanching spot larger than 2 millimeters. Both rashes are relatively common, especially in children, and they are a symptom of many different diseases and conditions, including enterovirus and meningitis.38
Causes and Risk Factors
What Causes Leukemia?
Leukemia is caused by genetic changes in bone marrow cells.5
Scientists have yet to determine what causes the genetic changes in bone marrow cells that lead to leukemia. However, certain risk factors are associated with the disease. For example, risk of leukemia increases with age, and the disease is most common in people over 60 years old.1,5
Leukemia and Genetics
The DNA inside of cells makes up a person’s genes, which control how those cells function. Genes called oncogenes help cells grow, divide, and stay alive while tumor suppressor genes control cell division and cause cells to die at the right time.6
Cells multiply by dividing into two cells, making a new copy of the chromosomes (strands of DNA). Sometimes errors occur during this process that affect genes in the new chromosomes, which can turn on oncogenes or turn off tumor suppressor genes.6
Several types of chromosome changes may contribute to leukemia and other types of cancer, including translocations—when DNA from one chromosome breaks off and becomes attached to a different chromosome, turning on oncogenes or turning off genes that would normally help a cell mature.6,7 For example, translocation of the so-called Philadelphia chromosome is present in ALL and CML. In this translocation, DNA is swapped between chromosomes 9 and 22.5,6
Other genetic mutations called deletions (the loss of part of a chromosome) might also cause certain types of leukemia. For example, people with CLL often have deletions in chromosomes 11, 13, and 17. Or they may have additions to chromosome 12.8
Not everyone with leukemia has the same genetic mutations even if they have the same type of leukemia. Some have multiple mutations, and others may have no known mutations.6
There are very few links between heredity and leukemia. Certain genetic syndromes can increase the risk of developing ALL and AML, but most leukemias are caused by gene mutations acquired after birth.1,5, 9,10
Leukemia Risk Factors
Certain demographic and lifestyle factors can increase the risk of leukemia. There are also environmental risk factors for leukemia. These risks vary based on the type of leukemia:
- Aging
Leukemia can occur at any age, but the risk increases with age for all types except ALL, which is more common in adults aged over 50 and children.9-12
- Sex
All leukemias are more common in those assigned male at birth than those assigned female.9-12
- Smoking
The only proven lifestyle-related risk factor for acute leukemias is smoking. This link has not been established for chronic leukemias.9-12
- Benzene exposure
The risk for acute leukemias increases if a person has been exposed to benzene—a solvent used in certain industries and found in cigarette smoke, gasoline, and motor vehicle exhaust as well as some glues, cleaning products, and art supplies.9-12
- Treatment with chemotherapy drugs
Chemotherapy drugs, specifically drugs called alkylating agents and topoisomerase II inhibitors, have been linked to a higher risk of AML.9 Chemotherapy also may increase the risk of ALL, and that risk may be elevated if combined with radiation therapy.10
- Radiation exposure
High doses of radiation (for example, from an atomic bomb blast or nuclear reactor accident) increase the risk for all leukemias except CLL, as does certain radiation therapy for cancer patients.9-12
- Certain blood disorders
People with chronic myeloproliferative disorders such as idiopathic myelofibrosis, polycythemia vera, and essential thrombocythemia may have an increased risk for AML.9
- Having a genetic syndrome
Some syndromes caused by hereditary genetic mutations could raise the risk for both acute leukemias:
- Bloom syndrome9
- Ataxia-telangiectasia9
- Diamond-Blackfan anemia9
- Fanconi anemia9
- Klinefelter syndrome10
- Li-Fraumeni syndrome9
- Shwachman-Diamond syndrome9
- Neurofibromatosis type 19
- Severe congenital neutropenia (Kostmann syndrome)9
- Certain chromosomal abnormalities
Trisomy 8 and Down syndrome increase the risk of AML.9 Down syndrome also increases the risk of ALL.10
- Family history
Although the links between heredity and leukemia seem to be minor, having an immediate relative with AML, CLL, or ALL increases the risk for the disease. The risk is higher for AML and ALL if someone has an identical twin who develops the disease before age 1.9,10,11
Leukemia Prevention
There is currently no known way to prevent most types of leukemia, especially among children. You can reduce some acute leukemia risk factors by avoiding smoking and contact with benzene.13
Diagnosis and Treatment
Leukemia Diagnosis
Doctors will collect information and medical samples to diagnose leukemia and determine which type and stage of leukemia is present.
- How Doctors Test for Leukemia
Doctors may use several tests to diagnose leukemia:1
- Medical history
- Physical exams
- Genetic tests to look for chromosome and gene changes
- Leukemia blood testing methods, such as a complete blood count
- Bone marrow tests, including bone marrow aspiration or biopsy, to gather tissue samples
- Once someone is diagnosed with leukemia, a healthcare provider may perform imaging tests and a lumbar puncture, or spinal tap, to determine if the cancer has spread.1
- How Acute Leukemias Are Staged
Most cancers are staged according to tumor size and how much the cancer has spread. This information helps determine prognosis and treatment decisions. But leukemia does not form tumors. Leukemia cells typically affect the bone marrow and may spread to nearby organs—most commonly, the liver and spleen—so it is not classified into traditional stages. Each type of leukemia is also classified differently.40
AML and ALL are classified based on the subtype of AML, lab tests, the patient's age, and other factors that help determine the outlook and treatment.40,41
Lab tests can help determine a patient’s leukemia subtype and prognosis. In 2016, the World Health Organization (WHO) created a new system that divides AML into 25 subtypes and ALL into 12 subtypes based on which genetic abnormalities are present, whether the cancer is related to previous cancer treatment, and other differentiating factors.40,41
- How Chronic Myeloid Leukemia Is Classified
The prognosis for CML depends on the phase of the disease and the number of blasts (immature white blood cells) in the bone marrow as well as other factors like blood counts, the age of the patient, and the presence of an enlarged spleen.42
CML is classified into three phases:42
- Chronic phase. Patients have less than 10% blasts in their blood and bone marrow samples and usually have fairly mild symptoms (if any). The majority of patients diagnosed with CML are in the chronic phase.
- Accelerated phase. Features of the accelerated phase include patients with blood samples that have 15% to <30% blasts, very low platelet counts not caused by treatment, or new chromosome changes in leukemia cells.
- Blast (or acute) phase. Patients have 20% or more blasts in their bone marrow/blood samples, and blasts have spread to tissues and organs.
- How Chronic Lymphocytic Leukemia Is Classified
There are two common systems for staging CLL:43
- Rai system. Most commonly used in the U.S., this classification includes five stages and is based on the number of blood cell counts and whether the cancer has spread. Stage 0 leukemia is low risk, stage 1 and stage 2 leukemia are intermediate risk, and stage 3 and stage 4 leukemia are high risk.
- Binet system. Most commonly used in Europe, this system classifies CLL into three stages—A, B, and C—based on the number of affected lymphoid tissues and whether the patient has too few red blood cells or blood platelets.
- How Chronic Myelomonocytic Leukemia Is Classified
CMML is divided into two groups based on bone marrow and blood cell counts:44
- CMML-1. Blasts are less than 5% of white blood cells and less than 10% of bone marrow cells.
- CMML-2. Blasts are 5% to 20% of white blood cells or 10% to 20% of bone marrow cells.
Leukemia Treatment
Leukemia treatment options vary based on the type of leukemia and how far it has spread. A doctor will also consider age, white blood cell count, and whether the patient was previously treated for cancer.45
Treatment options for leukemia include:
- Conventional chemotherapy. Systemic treatment that travels throughout the body and kills cancer cells.45
- A bone marrow transplant. This procedure replaces faulty bone marrow stem cells with healthy ones.1,46
- Radiation therapy. High doses of radiation attack and kill cancer cells.1,47
- Immunotherapy. These drugs enable the immune system to better fight cancer.48
- Splenectomy. The spleen is surgically removed.49
- Targeted therapy. These drugs attack specific cancer cells.1
Leukemia Complications
In rare cases, leukemia can cause serious complications that require immediate medical attention. For example, T cell ALL can cause enlargement of the thymus, a small organ located behind the sternum (breastbone) and in front of the trachea (windpipe). An enlarged thymus puts pressure on the trachea, which can cause trouble breathing or excessive coughing. It can also put pressure on the superior vena cava (SVC), a large vein that transports blood to the heart, causing blood to build up in the veins. This is a life-threatening condition called SVC syndrome, which can cause these symptoms:33
- Swelling in the neck, face, arms, and upper chest (sometimes with a bluish-red color)
- Headaches
- Dizziness
- Loss of consciousness

With AML, cancer cells are larger than normal white blood cells and may clog blood vessels and cause a condition called leukostasis, a rare but life-threatening medical emergency that causes stroke-like symptoms.39
Certain types of AML can also cause bleeding and clotting deficiencies, including dangerous blood clots that require immediate treatment.32
Global Impact of Leukemia

Worldwide, approximately 2.43 million people have leukemia.50 It is the 11th leading cause of cancer deaths, accounting for 3.2% of all new cancer cases and 3.9% of all cancer deaths.2 Because the disease is more common among older people, the burden of leukemia tends to be higher in developed countries than in developing middle- or low-income countries.51
Globally, leukemia places a large financial burden on individuals, families, insurers, and governments. In the U.S., for example, insurers spend an average of $200,000 to treat a person with chronic leukemia and $800,000 for a person with acute leukemia.52 A 2020 study estimated that the annual management cost for patients with for AML and myelodysplastic syndromes in Spain was €30,775 and €10,132 respectively. That’s about $31,895 and $10,500 at current exchange rates as of November 2022.53 A similar 2019 study in Sweden determined that total treatment cost, from a patient’s stem cell transplant until death, exceeded $160,000.54 A 2013 study in the Netherlands found that the average cost for an initial AML treatment alone was €117,495 in 2008 and 2009, or about $121,771 at current exchange rates as of November 2022.55
Learn More About Leukemia
Find a Pfizer leukemia clinical trial at PfizerClinicalTrials.com.
Explore leukemia clinical trials at ClinicalTrials.gov.
Area of Focus: Oncology
Leukemia is a focus area for Pfizer Oncology. To learn more about how we’re accelerating breakthroughs to outdo cancer, visit the Oncology page.
Find resources for those living with cancer and their caregivers at This is Living with Cancer.
- References
- Leukemia. MedlinePlus. https://medlineplus.gov/leukemia.html. Last updated September 1, 2021. Accessed February 15, 2022.
- Cancer stat facts: Leukemia. National Cancer Institute. https://seer.cancer.gov/statfacts/html/leuks.html. Accessed February 15, 2022.
- Siegel RL, Miller KD, Fuchs HE, et al. Cancer statistics, 2022. CA: A Cancer Journal for Clinicians. 2022;72(1):7-33. https://doi.org/10.3322/caac.21708. Published January 12, 2022. Accessed February 15, 2022.
- Facts and Statistics Overview. Leukemia & Lymphoma Society. https://www.lls.org/facts-and-statistics/facts-and-statistics-overview. Accessed June 3, 2022.
- What is acute lymphocytic leukemia (ALL)? American Cancer Society. https://www.cancer.org/cancer/acute-lymphocytic-leukemia/causes-risks-prevention/what-causes.html. Last revised October 17, 2018. Accessed February 15, 2022.
- What causes chronic myeloid leukemia? American Cancer Society. https://www.cancer.org/cancer/chronic-myeloid-leukemia/causes-risks-prevention/what-causes.html. Last revised June 19, 2018. Accessed February 15, 2022.
- Alberts B, Johnson A, Lewis J, Raff M, Roberts K, Walter P. Finding the cancer-critical genes. Molecular Biology of the Cell 4th edition. Published online 2002.
- Do we know what causes chronic lymphocytic leukemia? American Cancer Society. https://www.cancer.org/cancer/chronic-lymphocytic-leukemia/causes-risks-prevention/what-causes.html. Last revised May 10, 2018. Accessed February 15, 2022.
- Risk factors for acute myeloid leukemia (AML). American Cancer Society. https://www.cancer.org/cancer/acute-myeloid-leukemia/causes-risks-prevention/risk-factors.html. Last revised August 21, 2018. Accessed February 15, 2022.
- Risk factors for acute lymphocytic leukemia (ALL). American Cancer Society. https://www.cancer.org/cancer/acute-lymphocytic-leukemia/causes-risks-prevention/risk-factors.html. Last revised October 17, 2018. Accessed February 15, 2022.
- What are the risk factors for chronic lymphocytic leukemia? American Cancer Society. https://www.cancer.org/cancer/chronic-lymphocytic-leukemia/causes-risks-prevention/risk-factors.html. Last revised May 10, 2018. Accessed February 15, 2022.
- Risk factors for chronic myeloid leukemia. American Cancer Society. https://www.cancer.org/cancer/chronic-myeloid-leukemia/causes-risks-prevention/risk-factors.html. Last revised June 19, 2018. Accessed February 15, 2022.
- Questions and answers about leukemia. Centers for Disease Control and Prevention. https://www.cdc.gov/nceh/radiation/phase2/mleukemi.pdf. Accessed February 15, 2022.
- What is acute lymphocytic leukemia (ALL)? American Cancer Society. https://www.cancer.org/cancer/acute-lymphocytic-leukemia/about/what-is-all.html. Last revised October 17, 2018. Accessed November 17, 2022.
- Key statistics for acute lymphocytic leukemia (ALL). American Cancer Society. https://www.cancer.org/cancer/acute-lymphocytic-leukemia/about/key-statistics.html. Last revised January 12, 2022. Accessed February 15, 2022.
- What is acute myeloid leukemia (AML)? American Cancer Society. https://www.cancer.org/cancer/acute-myeloid-leukemia/about/what-is-aml.html. Last revised August 21, 2018. Accessed February 15, 2022.
- Treatment response rates for acute myeloid leukemia (AML). https://www.cancer.org/cancer/acute-myeloid-leukemia/treating/response-rates.html. Last revised August 21, 2018. Accessed October 10, 2022.
- Key statistics for acute myeloid leukemia. American Cancer Society. https://www.cancer.org/cancer/acute-myeloid-leukemia/about/key-statistics.html. Last revised January 12, 2022. Accessed February 15, 2022.
- What is chronic lymphocytic leukemia? American Cancer Society. https://www.cancer.org/cancer/chronic-lymphocytic-leukemia/about/what-is-cll.html. Last revised May 10, 2018. Accessed February 15, 2022.
- Key statistics for chronic lymphocytic leukemia. American Cancer Society. https://www.cancer.org/cancer/chronic-lymphocytic-leukemia/about/key-statistics.html. Last revised January 12, 2022. Accessed February 15, 2022.
- What is chronic myeloid leukemia? American Cancer Society. https://www.cancer.org/cancer/chronic-myeloid-leukemia/about/what-is-cml.html. Last revised June 19, 2018. Accessed February 15, 2022.
- Perrotti D, Jamieson C, Goldman J, Skorski T. Chronic myeloid leukemia: mechanisms of blastic transformation. J Clin Invest. 2010;120(7):2254-2264.
- CML phases and prognostic factors. Leukemia & Lymphoma Society. https://www.lls.org/leukemia/chronic-myeloid-leukemia/diagnosis/cml-phases-and-prognostic-factors. Accessed October 10, 2022.
- Key statistics for chronic myeloid leukemia. American Cancer Society. https://www.cancer.org/cancer/chronic-myeloid-leukemia/about/statistics.html. Last revised January 12, 2022. Accessed February 15, 2022.
- Chronic myeloid leukemia. Leukemia & Lymphoma Society. https://www.lls.org/research/chronic-myeloid-leukemia-cml. Accessed October 11, 2022.
- What is chronic myelomonocytic leukemia? American Cancer Society. https://www.cancer.org/cancer/chronic-myelomonocytic-leukemia/about/what-is-chronic-myelomonocytic.html. Last revised October 25, 2017. Accessed February 15, 2022.
- Key statistics about chronic myelomonocytic leukemia. American Cancer Society. https://www.cancer.org/cancer/chronic-myelomonocytic-leukemia/about/key-statistics.html. Last revised October 15, 2017. Accessed February 15, 2022.
- What is childhood leukemia? American Cancer Society. https://www.cancer.org/cancer/leukemia-in-children/about/what-is-childhood-leukemia.html. Last revised February 12, 2019. Accessed February 15, 2022.
- Cancer stat facts: Childhood leukemia (ages 0-19). National Cancer Institute. https://seer.cancer.gov/statfacts/html/childleuk.html. Accessed August 9, 2022.
- Risk of dying from cancer continues to drop at an accelerated pace. American Cancer Society. https://www.cancer.org/latest-news/facts-and-figures-2022.html. Published January 12, 2022. Accessed February 15, 2022.
- Key statistics for childhood leukemia. American Cancer Society. https://www.cancer.org/cancer/leukemia-in-children/about/key-statistics.html. Last reviewed January 12, 2022. Reviewed February 15, 2022.
- Signs and symptoms of acute myeloid leukemia (AML). American Cancer Society. https://www.cancer.org/cancer/acute-myeloid-leukemia/detection-diagnosis-staging/signs-symptoms.html. Last revised August 21, 2018. Accessed February 15, 2022.
- Signs and symptoms of acute lymphocytic leukemia (ALL). American Cancer Society. https://www.cancer.org/cancer/acute-lymphocytic-leukemia/detection-diagnosis-staging/signs-symptoms.html. Last revised October 17, 2018. Accessed February 15, 2022.
- Signs and symptoms of chronic myeloid leukemia. American Cancer Society. https://www.cancer.org/cancer/chronic-myeloid-leukemia/detection-diagnosis-staging/signs-symptoms.html. Last revised June 19, 2018. Accessed February 15, 2022.
- Signs and symptoms of chronic lymphocytic leukemia. American Cancer Society. https://www.cancer.org/cancer/chronic-lymphocytic-leukemia/detection-diagnosis-staging/signs-symptoms.html. Last revised May 10, 2018. Accessed February 15, 2022.
- Signs and symptoms of chronic myelomonocytic leukemia. American Cancer Society. https://www.cancer.org/cancer/chronic-myelomonocytic-leukemia/detection-diagnosis-staging/signs-symptoms.html. Last revised October 24, 2017. Accessed February 15, 2022.
- Signs and symptoms of childhood leukemia. American Cancer Society. https://www.cancer.org/cancer/leukemia-in-children/detection-diagnosis-staging/signs-and-symptoms.html. Last revised February 12, 2019. Accessed February 15, 2022.
- McGrath A, Barrett MJ. Petechiae. StatPearls.https://www.ncbi.nlm.nih.gov/books/NBK482331/. Last updated September 13, 2021. Accessed February 15, 2022.
- Ali AM, Mirrakhimov AE, Abboud CN, Cashen AF. Leukostasis in adult acute hyperleukocytic leukemia: a clinician’s digest: Leukostasis: a clinician’s digest. Hematol Oncol. 2016;34(2):69-78.
- Acute myeloid leukemia (AML) subtypes and prognostic factors. American Cancer Society. https://www.cancer.org/cancer/acute-myeloid-leukemia/detection-diagnosis-staging/how-classified.html. Last revised August 21, 2018. Accessed February 15, 2022.
- Acute lymphocytic leukemia (ALL) subtypes and prognostic factors. American Cancer Society. https://www.cancer.org/cancer/acute-lymphocytic-leukemia/detection-diagnosis-staging/how-classified.html. Last revised October 17, 2018. Accessed February 15, 2022.
- Phases of chronic myeloid leukemia. American Cancer Society. https://www.cancer.org/cancer/chronic-myeloid-leukemia/detection-diagnosis-staging/staging.html. Last revised June 19, 2018. Accessed February 15, 2022.
- How is chronic lymphocytic leukemia staged? American Cancer Society. https://www.cancer.org/cancer/chronic-lymphocytic-leukemia/detection-diagnosis-staging/staging.html. Last revised May 10, 2018. February 15, 2022.
- How is chronic myelomonocytic leukemia staged? American Cancer Society. https://www.cancer.org/cancer/chronic-myelomonocytic-leukemia/detection-diagnosis-staging/staging.html. Last revised October 24, 2017. Accessed February 15, 2022.
- How is chemotherapy used to treat cancer? American Cancer Society. https://www.cancer.org/treatment/treatments-and-side-effects/treatment-types/chemotherapy/how-is-chemotherapy-used-to-treat-cancer.html. Last revised November 22, 2019. Accessed October 11, 2022.
- Bone marrow transplantation. MedlinePlus. https://medlineplus.gov/bonemarrowtransplantation.html. Last revised April 17, 2017. Accessed November 17, 2022.
- Radiation therapy. MedlinePlus. https://medlineplus.gov/radiationtherapy.html. Last revised August 29, 2014. Accessed November 17, 2022.
- Immunotherapy. Leukemia & Lymphoma Society. https://www.lls.org/treatment/types-treatment/immunotherapy. Accessed October 11, 2022.
- Splenectomy. Leukemia & Lymphoma Society. https://www.lls.org/leukemia/chronic-lymphocytic-leukemia/treatment/splenectomy. Accessed October 11, 2022.
- Lin X, Wang J, Huang X, et al. Global, regional, and national burdens of leukemia from 1990 to 2017: A systematic analysis of the global burden of disease 2017 study. Aging. 2021;13(7):10468-10489. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8064161/. Published April 15, 2021. Accessed February 16, 2022.
- Yi M, Li A, Zhou L, et al. The global burden and attributable risk factor analysis of acute myeloid leukemia in 195 countries and territories from 1990 to 2017: Estimates based on the global burden of disease study 2017. Journal of Hematology and Oncology. 2020;13(72).
- Dieguez G, Ferro C, Rotter D. Milliman Research Report: The cost burden of blood cancer care: A longitudinal analysis of commercially insured patients diagnosed with blood cancer. The Leukemia and Lymphoma Society. https://www.lls.org/sites/default/files/Milliman%20study%20cost%20burden%20of%20blood%20cancer%20care.pdf. Published October 2018. Accessed February 16, 2022.
- Marsà A, Ascanio M, Diaz-García J, Darbà J. Epidemiology, management, and economic impact of acute myeloid leukemia and myelodysplastic syndrome in Spain at the hospital level: a claims database analysis. Journal of Medical Economics. 2020;23(12):1477-1484.
- Hernlund E, Redig J, Rangert Derolf Å, et al. Costs per treatment phase for AML patients receiving high-dose chemotherapy in Sweden. Blood. 2019;134(Supplement_1):2154-2154.
- Leunis A, Blommestein HM, Huijgens PC, Blijlevens NMA, Jongen-Lavrencic M, Uyl-de Groot CA. The costs of initial treatment for patients with acute myeloid leukemia in the Netherlands. Leukemia Research. 2013;37(3):245-250.
- Typical treatment of acute lymphocytic leukemia (ALL). American Cancer Society. https://www.cancer.org/cancer/acute-lymphocytic-leukemia/treating/typical-treatment.html. Last revised October 8, 2021. Accessed October 12, 2022.
- Typical treatment for acute myeloid leukemia (except APL). American Cancer Society. https://www.cancer.org/cancer/acute-myeloid-leukemia/treating/typical-treatment-of-aml.html. Last revised May 25, 2022. Accessed October 12, 2022.
- Living as a chronic lymphocytic leukemia survivor. American Cancer Society. https://www.cancer.org/cancer/chronic-lymphocytic-leukemia/after-treatment/follow-up.html. Last revised May 10, 2018. Accessed October 12, 2022.
- Treatment outcomes. Leukemia & Lymphoma Society. https://www.lls.org/leukemia/chronic-myeloid-leukemia/treatment/treatment-outcomes. Accessed October 12, 2022.
- Diaz Duque A, Cabrero M, Ravandi F, et al. Long-term outcome of chronic myelomonocytic leukemia (CMML) patients treated with hypomethylating agents (Hma): a single-institution experience. Blood. 2014;124(21):1924-1924.
- Hematologist. National Cancer Institute. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/hematologist. Accessed November 17, 2022.
- Oncologist. National Cancer Institute. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/oncologist. Accessed November 17, 2022.
- Your treatment team. Leukemia and Lymphoma Society. https://www.lls.org/treatment/your-treatment-team. Accessed November 17, 2022.
The information contained on this page is provided for your general information only. It is not intended as a substitute for seeking medical advice from a healthcare provider. Pfizer is not in the business of providing medical advice and does not engage in the practice of medicine. Pfizer under no circumstances recommends particular treatments for specific individuals and in all cases recommends consulting a physician or healthcare center before pursuing any course of treatment.
Related Articles
Cancer Screenings: Understanding the Pros and Cons
Cancer screenings can be powerful tools that can help find the disease at an early stage, when it may be easier to treat. Most of the time screenings do not diagnose cancer. Instead, they help your healthcare provider see if you need more tests. For example, a mammogram may find a breast lump, but a...
Living with Chronic Myeloid Leukemia (CML)
Chronic myeloid (or myelogenous) leukemia (CML) is one of four main types of leukemia that can affect adults. These 4 types of leukemia are classified as either myeloid or lymphocytic based on the type of cells affected, and either acute or chronic. The chronic forms of leukemia tend to take longer...
Tackling the Complex Challenges of Hard-to-Treat Blood Cancers
Blood cancers remain one of the greatest health challenges of our lifetime. In 2020, more than 1 million people worldwide were diagnosed with a blood cancer.[1] And while no two blood cancers are alike – whether leukemia, lymphoma, or myeloma -- treatments vary greatly.[2] What Makes Blood Cancers...




